Radiculopathy Rehab: What Works, What to Avoid, and How to Stay Consistent
When a spinal nerve gets squeezed—whether by a herniated disc, bone spur, or swelling—you get radiculopathy, a condition where a pinched nerve root causes pain, tingling, or weakness that shoots down the arm or leg. Also known as sciatica when it affects the lower back and leg, it’s not just a back problem—it’s a nerve problem that changes how you move, sit, and sleep. This isn’t something you wait out. Without the right rehab, nerve irritation can turn into chronic pain, muscle loss, or even permanent weakness.
Physical therapy for radiculopathy, a structured, movement-based approach to reduce nerve pressure and restore function is the most proven path forward. It’s not about brute force stretching or aggressive massage. It’s about gentle, controlled motion that teaches your body to stop guarding the area. Things like nerve glides—simple movements that let the nerve slide freely through its tunnel—can make a bigger difference than pills. And core stability? It’s not about six-pack abs. It’s about training your deep abdominal and back muscles to take pressure off the spine so the nerve isn’t constantly being pinched.
People often skip rehab because they feel better after a few days. But radiculopathy flares up again because the root cause—poor movement patterns, weak muscles, or tight tissues—was never fixed. That’s why consistency beats intensity. Doing 10 minutes of the right exercises every day works better than one hour once a week. And it’s not just about exercises. Sitting for long periods? That’s a trigger. Poor posture at your desk? That’s a risk. Even sleeping on a mattress that doesn’t support your spine can undo progress.
Spinal nerve compression, the mechanical pressure causing radiculopathy symptoms doesn’t always show up on an MRI. Sometimes, the nerve is fine on the scan but still irritated from daily habits. That’s why rehab focuses on function, not just images. You might have a bulging disc and no pain—or a perfectly clean scan and crippling discomfort. The goal isn’t to fix the disc. It’s to fix how you use your body so the disc doesn’t keep bothering the nerve.
And don’t assume surgery is the next step. Most cases improve with rehab alone. But if you’ve tried physical therapy for 6-8 weeks and still can’t walk without pain, lift your leg, or sleep through the night, then it’s time to talk to a specialist. But even then, rehab stays part of the plan—before and after.
What you’ll find below aren’t just generic stretches. These are real posts from people who’ve been there: how to adjust your workout when you have nerve pain, why some exercises make it worse, how to tell if your pain is coming from the nerve or just a muscle, and what to do when meds stop helping. You’ll see how people rebuilt movement after months of pain, what tools actually helped, and the mistakes that cost them time. No fluff. No hype. Just what works when your body says no.
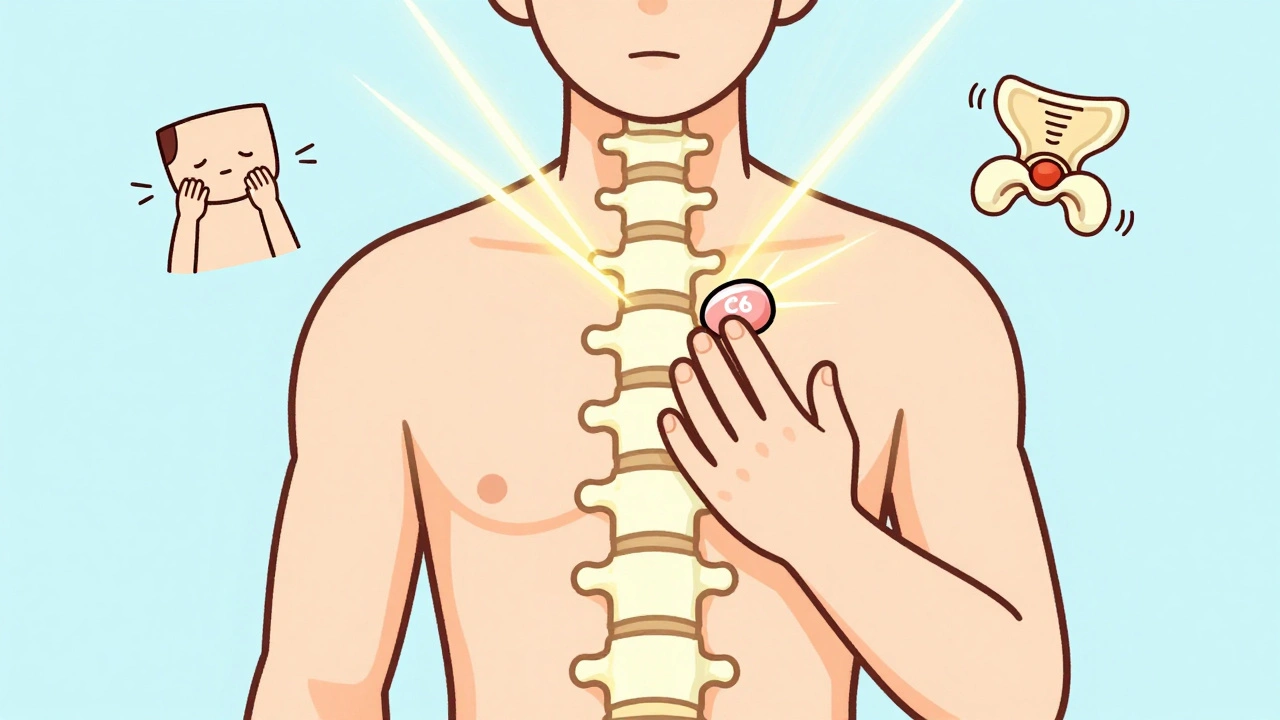
Cervical and Lumbar Radiculopathy: Nerve Pain and Rehabilitation That Actually Works
Cervical and lumbar radiculopathy cause nerve pain that shoots into arms or legs. Most cases improve with targeted rehab, not surgery. Learn what actually works, what doesn't, and how to recover faster.
View More