
Antacid-Antibiotic Timing Calculator
Antacid & Antibiotic Interaction Calculator
Enter your antibiotic and antacid to calculate the safe separation time to ensure your antibiotic works effectively.
Recommended Timing
Critical Warning
Many people reach for an OTC antacid like Tums, Maalox, or Mylanta when they feel heartburn or indigestion. It’s quick, easy, and works fast. But if you’re also taking an antibiotic - say, for a sinus infection, UTI, or pneumonia - you could be sabotaging your treatment without even knowing it.
Why Antacids Kill Antibiotic Effectiveness
OTC antacids don’t just neutralize stomach acid. They contain metal ions - aluminum, magnesium, calcium - that latch onto certain antibiotics like a magnet. This forms a tight, insoluble bond called a chelate. Once that happens, your body can’t absorb the antibiotic properly. The drug passes through your gut and out of your system, useless.This isn’t theoretical. Studies show tetracycline antibiotics (like doxycycline) can lose up to 90% of their absorption when taken with an aluminum-based antacid. Fluoroquinolones like ciprofloxacin and levofloxacin drop by 50-75%. Even amoxicillin, often thought to be safe, sees an 18-22% reduction in absorption when mixed with common antacids.
The problem isn’t the acid itself. It’s the metal. Antacids with aluminum hydroxide or magnesium hydroxide are the worst offenders. Calcium carbonate (the main ingredient in Tums) is also a major player. Sodium bicarbonate? Less of a concern for antibiotics, but it can still mess with other drugs.
Which Antibiotics Are Most at Risk?
Not all antibiotics are equally affected. Some are hit hard. Others barely notice. Here’s what the data says:- Tetracycline and doxycycline: Absorption drops 70-90%. These drugs are especially vulnerable because their chemical structure grabs onto metal ions like they’re made for it.
- Ciprofloxacin and levofloxacin: Bioavailability plummets from 70% down to 15-25% when taken with antacids. This is a big deal - it’s why some UTIs won’t clear up, even with the right antibiotic.
- Amoxicillin: Mixed results. Some studies show a modest 18-22% drop. Others show no effect, especially with amoxicillin-clavulanate. Still, it’s not worth the risk.
- Penicillins, cephalosporins, azithromycin: Minimal to no interaction. These are safer choices if you need both acid relief and antibiotics.
If your prescription is for doxycycline or ciprofloxacin, you’re in the danger zone. And if you’re taking antacids daily - even just one or two tablets - you’re likely reducing your antibiotic’s power without realizing it.
The Timing Trick That Saves Your Treatment
The good news? This interaction is avoidable. You don’t have to choose between comfort and cure. You just need to space things out.Medical guidelines agree: separate your antacid and antibiotic by at least 2 hours. But here’s the catch - it’s not the same for every drug.
- For tetracyclines and doxycycline: Take the antibiotic at least 2 hours before or 4 hours after the antacid.
- For fluoroquinolones like ciprofloxacin: Wait 4-6 hours after taking the antacid before taking your antibiotic. Some experts say even 8 hours is safer.
- For amoxicillin: If you’re unsure, stick with a 2-hour gap. It’s conservative and effective.
Why the difference? It’s about how long the antibiotic stays in your system and how quickly the antacid clears out. Fluoroquinolones are absorbed quickly in the upper gut, right where antacids are still working. Tetracyclines need a slightly acidic environment to dissolve - and antacids wipe that out.
Practical tip: Take your antibiotic first thing in the morning on an empty stomach. Wait 4 hours before reaching for an antacid. Or, if you take your antibiotic at night, avoid antacids after dinner until the next morning.

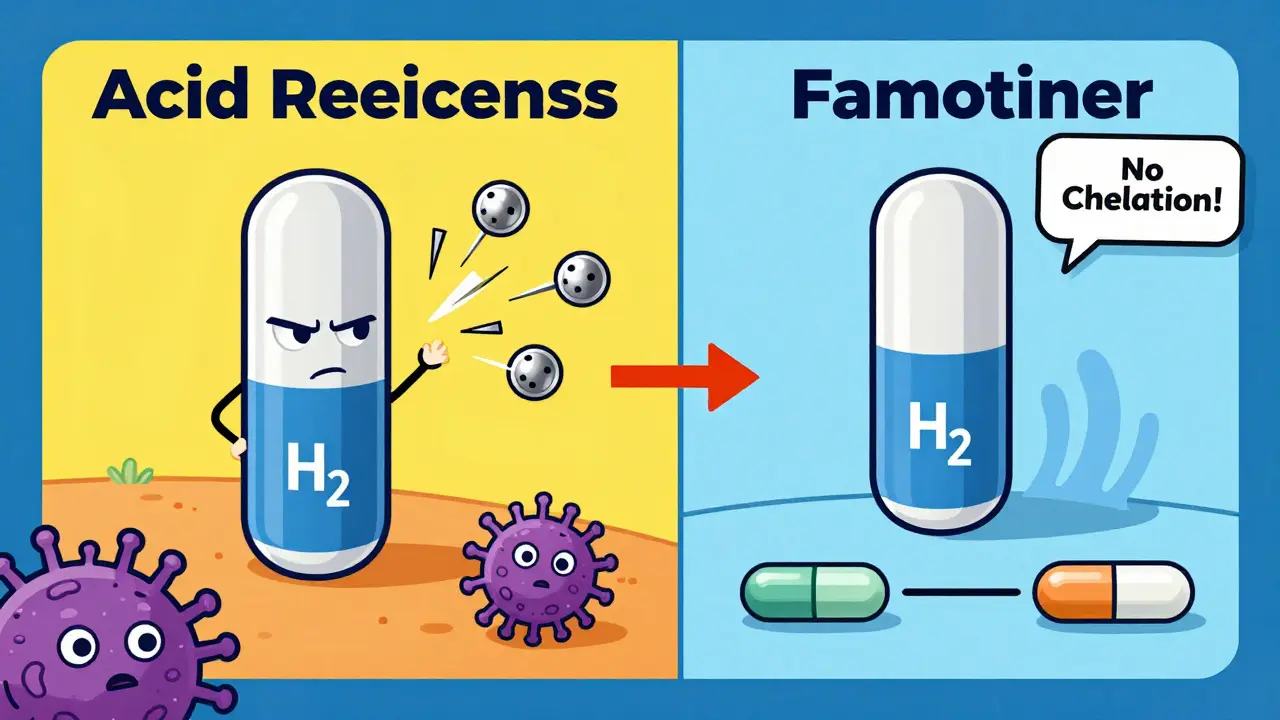
What About PPIs and H2 Blockers?
You might be thinking: “Why not just switch to omeprazole or famotidine?”That’s smarter than you think.
Proton pump inhibitors (PPIs) like omeprazole and H2 blockers like famotidine reduce acid production - they don’t neutralize it with metal ions. So they don’t form chelates. That makes them safer to use with antibiotics.
But there’s a trade-off: they take longer to work. PPIs can take 1-4 hours to start helping. H2 blockers kick in in 30-60 minutes. Antacids? 1-5 minutes.
If you need fast relief and are on a tetracycline or fluoroquinolone, you’re stuck. You can’t have both immediate comfort and full antibiotic power. You have to pick one. For most people, that means choosing the antibiotic - because treatment failure leads to longer illness, stronger infections, and even antibiotic resistance.
Real Consequences: When It Goes Wrong
This isn’t just a theory. People are getting sicker because of this.A 2023 case study from University Hospitals described a woman with recurring UTIs. She was prescribed ciprofloxacin three times. Each time, the infection came back. Why? She was taking Tums daily for heartburn. Her urine cultures kept showing the same bacteria. Only after her pharmacist asked about her antacid use - and she stopped taking it during treatment - did the infection clear for good.
A 2023 meta-analysis found that when antibiotics and antacids were taken together without spacing, treatment failure rates jumped by 37%. That’s nearly 4 out of 10 people not getting better because of a simple timing mistake.
And it’s getting worse. The CDC says over 35,000 Americans die each year from antibiotic-resistant infections. Incomplete antibiotic dosing - like what happens when antacids block absorption - is one of the biggest drivers of resistance. Your body doesn’t kill all the bacteria. The survivors get stronger. Next time, the same drug won’t work.
Who’s at Highest Risk?
This interaction hits harder for some people:- Elderly patients: More likely to take multiple meds, including antacids daily. Often don’t realize the interaction exists.
- People with GERD or chronic heartburn: May take antacids several times a day, every day. They don’t think twice about popping one with their antibiotic.
- Those on long-term antibiotics: Like doxycycline for acne or ciprofloxacin for chronic infections. Daily antacid use = daily interference.
A 2022 survey found only 32% of OTC antacid users knew about this risk. Even though the FDA required warning labels on packaging in 2019, a 2022 audit found only 67% of major brands followed through.
Pharmacists are on the front lines. In retail pharmacies, they’re often the last line of defense before a patient takes their antibiotic with a Tums. Yet many patients never even ask.
What You Should Do Right Now
If you’re taking an antibiotic and using OTC antacids, here’s what to do:- Check your antibiotic name. Is it doxycycline, tetracycline, ciprofloxacin, or levofloxacin? If yes, you’re at high risk.
- Look at your antacid. Does it list aluminum hydroxide, magnesium hydroxide, or calcium carbonate? If yes, you’re in danger zone.
- Separate them. Take your antibiotic at least 2 hours before or 4-6 hours after your antacid. Don’t guess - time it.
- Ask your pharmacist. Bring both bottles. They’ll tell you exactly how to space them.
- Consider alternatives. If you need daily acid relief, talk to your doctor about switching to famotidine or omeprazole - even temporarily - while on antibiotics.
- Don’t skip doses. If you forget to space them, take your antibiotic anyway. But don’t repeat the mistake. Write it down.
Remember: Antacids aren’t evil. They’re helpful. But they’re not safe with every drug. Timing matters. And your recovery depends on it.
What If You Already Took Them Together?
If you accidentally took your antibiotic and antacid at the same time - don’t panic. Don’t double up on your antibiotic dose. That’s dangerous.Just skip your next antacid dose until you’ve waited the full 4-6 hours. Resume your normal schedule after that. One mistake won’t ruin your treatment - but doing it every day might.
Keep a small note on your phone: "Antibiotic → wait 4 hours → antacid." Set a reminder if you need to. It’s that simple.
Can I take Tums with amoxicillin?
It’s not recommended. While some studies show little to no effect on amoxicillin, others show a 18-22% drop in absorption when taken with aluminum-magnesium antacids. Since the risk isn’t zero and the fix is simple - just wait 2 hours - it’s safer to avoid combining them. If you’re unsure, ask your pharmacist.
How long should I wait after taking an antacid before taking doxycycline?
Wait at least 4 hours after taking an antacid before taking doxycycline. The reverse is also true: take doxycycline at least 2 hours before any antacid. This gap gives the antibiotic time to absorb before the antacid changes the chemistry in your gut.
Are all antacids equally bad with antibiotics?
No. Antacids with aluminum, magnesium, or calcium are the worst. Sodium bicarbonate (like Alka-Seltzer) has less impact on antibiotics. But even then, it’s not risk-free. Avoid all antacids with metal ions when taking tetracyclines or fluoroquinolones. If you’re unsure, check the active ingredients on the label.
Can I use antacids if I’m on penicillin?
Penicillin-based antibiotics like amoxicillin and ampicillin are less affected than tetracyclines or fluoroquinolones. Still, some studies show a small drop in absorption. To be safe, separate them by 2 hours. If you’re on a long course of antibiotics and have frequent heartburn, ask your doctor about switching to an H2 blocker like famotidine instead.
Why do pharmacists always ask about antacids when I pick up my antibiotic?
Because this is one of the most common and dangerous OTC-prescription drug interactions. The American Pharmacists Association lists it as the #3 most frequent interaction in their 2023 safety report. Pharmacists are trained to catch this - and they’re your best chance at avoiding a failed treatment.
What’s the safest acid reducer to use with antibiotics?
H2 blockers like famotidine (Pepcid) or ranitidine (if available) are safer than antacids because they don’t contain metal ions. Proton pump inhibitors like omeprazole are also safer. Neither causes chelation. But they take longer to work. If you need fast relief, you’ll have to time your antacid carefully - or accept that you’ll wait a bit longer for heartburn relief.
If you’re taking antibiotics for anything serious - a UTI, pneumonia, or skin infection - don’t gamble with your recovery. Antacids are convenient. But they’re not worth the risk if they make your antibiotic useless. Space them out. Talk to your pharmacist. Your body will thank you.






Faisal Mohamed
January 25 2026
Bro, this is peak bioavailability warfare 🧠💊. The chelation dynamic between divalent cations and quinolone scaffolds is basically a molecular hostage situation. Your gut’s just a passive observer while Ca²⁺ and Al³⁺ hijack your doxy like it’s a Netflix account. We’re not talking about minor pharmacokinetic noise - we’re talking about subtherapeutic AUCs leading to resistance Darwinism. 🤯