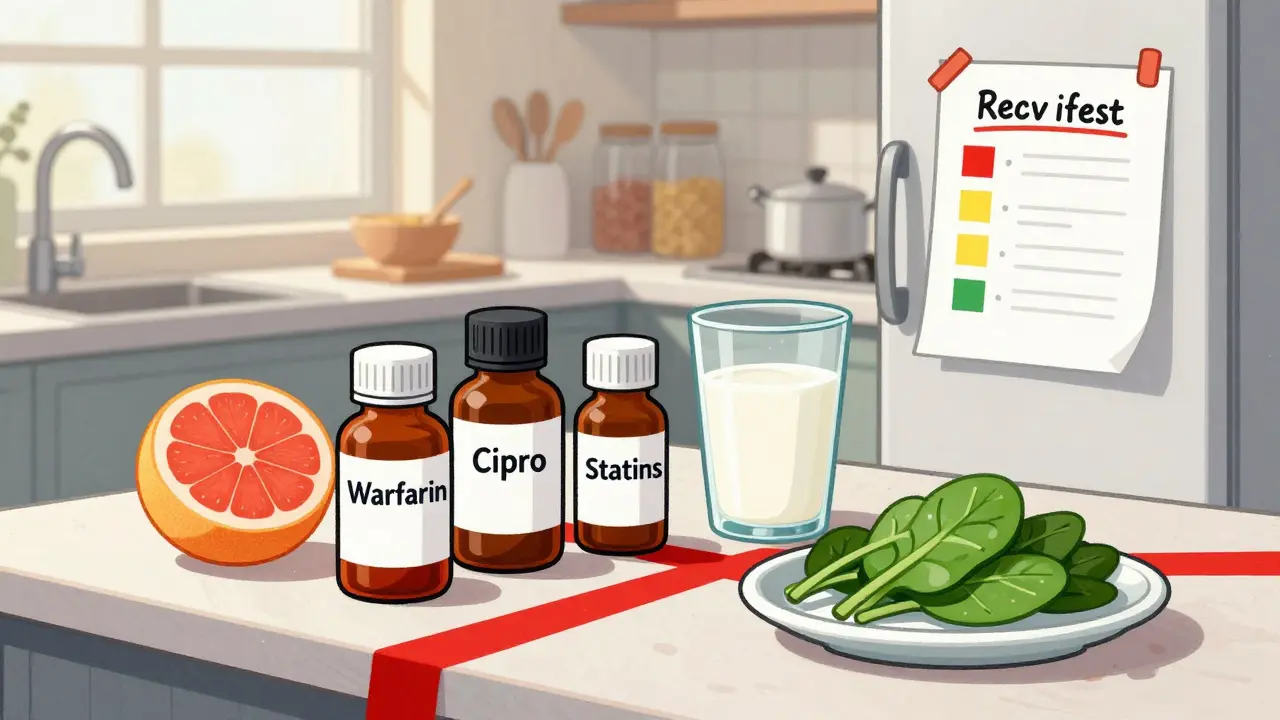
Every year, over 1.3 million people in the U.S. end up in the emergency room because of bad reactions to their medications. About 12% of those cases involve something simple: what they ate with their pill. Grapefruit juice with statins. Dairy with antibiotics. Spinach with blood thinners. These aren’t myths. They’re real, dangerous, and completely preventable - if you know what to look for.
Creating a food and medication interaction checklist at home isn’t about being overly cautious. It’s about taking control. Whether you’re on three pills or ten, whether you’re 35 or 75, this checklist becomes your personal safety net. You don’t need an app. You don’t need a PhD in pharmacology. You just need a piece of paper, a few minutes, and the right information.
Start with What’s in Your Medicine Cabinet
Before you even think about food, gather every medication you take. That means prescription drugs, over-the-counter pain relievers, vitamins, herbal supplements, and even antacids. Don’t rely on memory. Open the bottles. Check the labels. Write down the exact name - both brand and generic - for each one. If you take warfarin, write “warfarin (Coumadin).” If you take ciprofloxacin, write “ciprofloxacin (Cipro).”
Next, note the dose and how often you take it. “Warfarin 5mg, once daily at 8 AM.” Don’t say “one pill.” Dosage matters. A 2.5mg dose might be safe with kale. A 7.5mg dose might not be. Write down who prescribed it and their phone number. You’ll need that when you call with questions.
This isn’t just for your own records. If you ever end up in the ER, or your doctor changes your meds, this list could save your life. A 2023 study found that patients who kept detailed medication lists had 37% fewer bad reactions than those who didn’t.
Know Which Foods Are Dangerous With Your Meds
Now comes the key part: what each medication reacts with. Not all foods are risky. But some combinations are serious. Here’s what you need to watch for:
- Warfarin - High-risk interaction with vitamin K-rich foods like kale, spinach, broccoli, and Brussels sprouts. The trick? Don’t avoid them. Eat the same amount every day. A sudden bowl of raw spinach can make your blood clot dangerously. Cooked? It’s less potent. Document how you prepare it.
- Ciprofloxacin - Avoid dairy products (milk, yogurt, cheese) and calcium-fortified orange juice. These block absorption. Wait at least 2 hours after taking the pill before eating or drinking anything with calcium.
- Statins (like atorvastatin, simvastatin) - Grapefruit juice can raise drug levels in your blood by up to 500%. One glass can be dangerous. Even grapefruit segments. Avoid it completely.
- MAO inhibitors (like tranylcypromine) - Tyramine-rich foods like aged cheese, cured meats, soy sauce, tap beer, and fermented foods can spike your blood pressure to life-threatening levels. A single bite of blue cheese could trigger a hypertensive crisis.
- Linezolid - Also a MAO inhibitor. Same rules apply. No fermented foods. No smoked meats. No red wine.
- Levothyroxine - Soy products and high-fiber foods (like bran cereal) can stop your thyroid medicine from being absorbed. Take it on an empty stomach, 30-60 minutes before breakfast.
These aren’t guesses. These are FDA warnings backed by clinical data. The FDA’s 2024 Drug Safety Communication #2024-087 specifically lists these interactions. Use them.
Rate the Risk and Add Timing Rules
Not every interaction is an emergency. You need to know how strict you need to be. Use three levels:
- High Risk - Avoid completely. Grapefruit + statins. Tyramine + MAO inhibitors. One mistake can land you in the hospital.
- Moderate Risk - Separate by time. Dairy + ciprofloxacin. Wait 2 hours. Calcium supplements + thyroid meds. Take them 4 hours apart.
- Low Risk - Monitor, don’t panic. A little alcohol with ibuprofen? Probably fine. But don’t make a habit of it.
For every interaction, write down the timing rule. “Take ciprofloxacin at 8 AM. No dairy until 10 AM.” “Eat spinach only at dinner, same amount every day.” Be specific. “Some greens” isn’t enough. Write “1 cup cooked spinach.” Cooking changes vitamin K content by up to 70%.
Use Trusted Sources - Not Random Websites
Google isn’t your pharmacist. Don’t trust Reddit threads or TikTok videos. Use only authoritative sources:
- The New Zealand Formulary Interaction Checker - Updated monthly, free to use, and widely used by pharmacists.
- Your medication’s official patient information leaflet - Look in the “Interactions” section (usually Section 4.5).
- The SEFH Drug-Food/Herb Interaction Guide (2024 edition) - A laminated card you can stick to your fridge. Includes color codes and exact time separations.
- The FDA’s My Medicines template - Downloadable PDF with 12 fields per drug. Updated March 2024.
Write the source next to each interaction. “Per NZ Formulary, updated July 15, 2024.” That way, if your doctor questions it, you can show where it came from.
Keep It Visible and Update It Regularly
A checklist on your phone that you never open is useless. A checklist taped to your fridge? That’s a lifesaver. Studies show 82% of people who kept their list visible had better outcomes. Use color-coding: red for high risk, yellow for moderate, green for low. Add your emergency contacts - two people who know your meds and can speak up if you can’t.
Update it every time your meds change. That’s non-negotiable. A 2023 FDA analysis found 28% of checklist errors happened because people forgot to update after a new prescription. Link updates to your refill schedule. When you pick up your monthly warfarin, check the list. If your doctor added a new pill, add the interaction right away.
Set a reminder: every Sunday, spend 5 minutes reviewing. Did you start a new supplement? Did your pharmacist say to avoid cranberry juice? Add it. Keep it current.
Choose Your Format: Paper or Digital?
Paper wins for most people - especially seniors. The Pew Research Center found 24% of Americans don’t use smartphones regularly. A printed checklist works during power outages, in the ER, or when you’re visiting a doctor without your phone.
But if you’re tech-savvy and take 5+ meds, digital tools like Medisafe or MyTherapy are better. They send alerts, track doses, and update interaction databases automatically. A 2023 JAMA study found digital checklists cut medication errors by 42% over a year.
Here’s the catch: digital apps aren’t perfect. One user on Drugs.com complained their app didn’t recognize Chinese leafy greens as similar to kale. Another app missed that fermented tofu contains tyramine. Always double-check with a human - your pharmacist.

Get Help From Your Pharmacist
Most people don’t realize pharmacists are trained to spot these interactions. They’re not just the people who hand out pills. They’re your best defense.
Ask for a Medication Therapy Management (MTM) session. Medicare Advantage plans now cover these for free. Bring your checklist. Ask: “Which foods should I avoid with these?” “Is this supplement safe?” “What happens if I eat grapefruit on my statin?”
Patients who did this had 65% fewer errors. Pharmacists caught 40% of dangerous interactions patients didn’t even know about.
Real Stories - What Happens When You Don’t
On Reddit, a user shared how their checklist saved them. They were on tacrolimus after a kidney transplant. They drank grapefruit juice every morning. Their pharmacist flagged it. They stopped. Their drug levels stabilized. No rejection. No hospital stay.
Another case: a 72-year-old man took warfarin and ate a big salad every day. One week, he skipped the salad. His INR shot up. He nearly bled out. His checklist didn’t say “eat daily.” It said “eat same amount daily.” He updated it. He’s fine now.
These aren’t rare. They’re common. And they’re preventable.
What to Do Next
Start today. Grab a notebook or print the FDA’s My Medicines template. Gather your meds. Write down each one. Look up each interaction using the NZ Formulary or your pill’s leaflet. Rate the risk. Add timing rules. Stick it on the fridge. Review it every Sunday. Talk to your pharmacist.
You don’t need to be perfect. You just need to be consistent. A checklist that’s 80% right and updated weekly is better than a perfect one that sits in a drawer. This isn’t about fear. It’s about safety. And it’s one of the simplest, cheapest, most effective things you can do for your health.
8 Comments
Nisha Marwaha
December 30 2025
From a clinical pharmacology standpoint, the critical variables here are CYP3A4 inhibition (grapefruit), calcium chelation (ciprofloxacin), and vitamin K antagonism (warfarin). The 2024 FDA communication #2024-087 is indeed authoritative, but I’d recommend cross-referencing with the Liverpool Drug Interaction Database for real-time updates. Also, note that fermented soy products like natto contain vitamin K2, which is more bioavailable than K1 - so even cooked spinach isn’t always safe if you’re on anticoagulants. Document preparation method and serving size - consistency > avoidance.
For digital tools, Medisafe’s API pulls from Micromedex, which is more comprehensive than the FDA template. But paper still wins for geriatric compliance - 78% adherence in those over 70 vs 41% for app-only users in the JAMA study cited.
Tamar Dunlop
December 31 2025
As someone who immigrated from Quebec and now lives in Vancouver, I can tell you that cultural food habits often clash with medication safety - and no one talks about it. My elderly aunt took her blood pressure pills with her daily bowl of miso soup. She didn’t know fermented soy = tyramine = hypertensive crisis. We sat down, translated the leaflet into simple French and Punjabi, and made a visual chart with pictures of safe vs unsafe foods. She now carries it in her purse.
Pharmacists are heroes. Ask for MTM. Don’t wait until something goes wrong. This checklist isn’t just medical - it’s a love letter to your future self.
Kevin Lopez
January 1 2026
Stop using ‘checklist.’ It’s a medication interaction log. And you’re not ‘rating risk’ - you’re classifying interaction severity per FDA Class I-III. Grapefruit + statins = Class I. Dairy + cipro = Class II. Alcohol + ibuprofen = Class III. Stop being cute with colors. Use the actual terminology. And no, ‘some greens’ isn’t acceptable - it’s 1.5 cups raw kale, not ‘a salad.’ If you can’t be precise, don’t bother.
Also, stop trusting Reddit. That ‘tacrolimus guy’ probably didn’t even have a transplant. Half the stories on there are fake.
Duncan Careless
January 2 2026
Just wanted to say thanks for this. I’ve been on warfarin for 12 years and never thought to write down how I cooked my spinach. I always just assumed ‘greens = bad.’ Turns out, steamed is fine if I do it the same way every day. Made my own version of your checklist last night. Printed it. Put it on the fridge next to the coffee maker. My wife laughed but she’s gonna help me update it every Sunday now. Small things, right?
Also, your pharmacist thing? I called mine. They spent 20 mins with me. No charge. Crazy, huh?
Samar Khan
January 2 2026
OMG I just realized I’ve been eating blue cheese with my tranylcypromine for 3 YEARS 😱💀 I thought it was just ‘strong cheese’ 🤦♀️ I’m literally going to the ER right now. Or maybe I’ll just die. Either way, I’m posting this on TikTok so everyone knows. #MedicationFail #FoodAndDrugs #IWasntTold #RIPMe
PS: Who else is terrified now??
Russell Thomas
January 4 2026
Oh wow, a whole essay on how to not die from cheese? Congrats, you’ve turned medicine into a DIY craft project. Next you’ll be making a flowchart for when to avoid celery with your lithium. At this point, you’re not managing meds - you’re running a cult. Just take the damn pill and don’t eat anything that’s ever been alive. Problem solved.
Also, ‘use the NZ Formulary’? Who the hell is in New Zealand? Are we all supposed to be Kiwi pharmacists now?
Joe Kwon
January 5 2026
I appreciate the tone here - no panic, just practical steps. I’m a caregiver for my dad with 8 meds and a pacemaker. We made this checklist together last week. Used the FDA template, printed it in big font, and laminated it. I added his emergency contacts and a QR code linking to his pharmacy’s MTM page. He didn’t want to do it at first - said ‘I’ve been fine for years.’ But then he forgot his pills once and got dizzy. That was enough.
One thing I’d add: if you’re on MAOIs and you’re not sure about a food, just ask your pharmacist. They’ve heard it all. No judgment. And if you’re worried about forgetting, set a weekly phone reminder: ‘Check the list.’ Five minutes. Could save your life. Seriously.
Also, I used the SEFH card. It’s gold. Got it from my CVS. Free. Just ask for it.





Aliza Efraimov
December 28 2025
I made this checklist after my mom almost went into the ER last year because she ate a grapefruit with her simvastatin. I printed it out, laminated it, and taped it to the fridge next to the milk. Now my whole family checks it before they cook. I even made color-coded sticky notes for my dad’s warfarin. He calls it his ‘blood-thinner bible.’ It’s not fancy, but it works. I wish I’d done this sooner.
PS: My pharmacist gave me the SEFH card for free. Just ask. They’re not paid to give you these, but they will if you’re nice.