When your neck or lower back sends sharp, shooting pain down your arm or leg, it’s not just a bad ache-it’s your nerve screaming for help. This is radiculopathy, a condition where a nerve root gets pinched or irritated as it leaves your spine. It’s not rare. In fact, about 1 in 5 adults will deal with it at some point, and most of those cases happen in the neck (cervical) or lower back (lumbar). The good news? Most people get better without surgery-if they know what to do and what not to do.
What Exactly Is Radiculopathy?
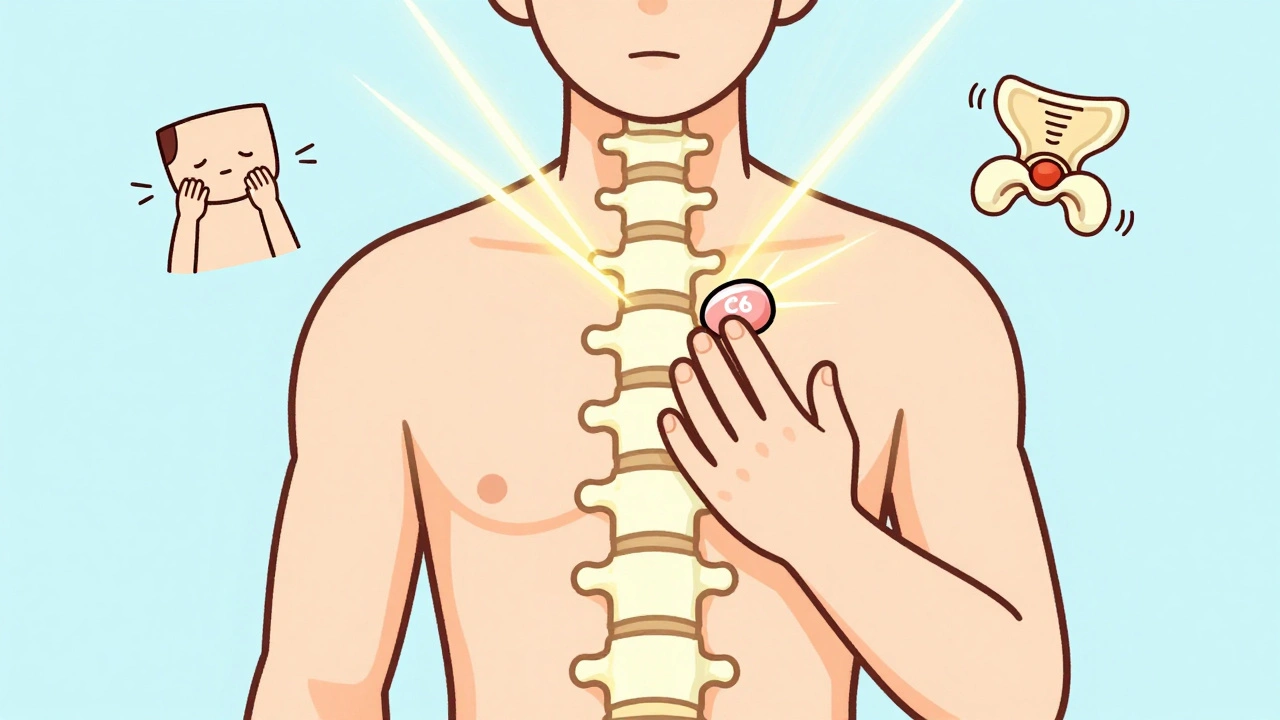
Radiculopathy isn’t a disease. It’s a symptom. Something is pressing on or irritating a nerve as it exits your spine. In the neck, that’s cervical radiculopathy. In the lower back, it’s lumbar radiculopathy-often called sciatica when it shoots down the leg. The nerve doesn’t just hurt where it’s squeezed. It sends pain, tingling, numbness, or weakness along its entire path. That’s why a pinched nerve in your neck can make your thumb go numb, or one in your lower back can cause your foot to drag. The most common causes? For people under 50, it’s usually a herniated disc. For those over 50, it’s more often bone spurs or narrowing of the space where the nerve exits-the technical term is foraminal stenosis. Trauma, heavy lifting, even poor posture over time can trigger it. MRI scans today can spot these problems with 92% accuracy, so doctors don’t have to guess anymore.Cervical vs. Lumbar: Where the Pain Goes
Not all nerve pain is the same. Where it starts tells you exactly which nerve is involved-and what to expect. In the neck, the most common culprits are C6 and C7 nerves. If C6 is pinched, you’ll feel pain along your thumb and index finger, and your biceps might feel weak. C7? That’s the middle finger and triceps weakness. C8 affects your ring and pinky fingers, making it hard to grip things. These patterns are so consistent that doctors can often guess the problem just by asking where you feel it. Down below, lumbar radiculopathy follows its own map. L5 nerve compression causes pain from your outer calf to your big toe, and you might notice your foot dropping when you walk. S1 nerve issues hit the back of your calf and the sole of your foot, making it hard to stand on your toes. These aren’t random symptoms-they’re the nerve’s way of saying, “I’m being squeezed here.”Why Lumbar Radiculopathy Feels Worse
Many people assume neck pain is the worst. But data shows lumbar radiculopathy tends to be more disabling. People with lower back nerve compression report 37% higher disability scores than those with neck issues. Recovery takes longer too-on average, 14 weeks versus 11 for cervical cases. Why? For one, your lower back carries your whole body weight. Every step, every twist, every lift puts pressure on those nerves. Plus, the nerves in your lower back are longer and more exposed, making them harder to protect. Work plays a big role. Construction workers, nurses, and warehouse staff are 3 times more likely to develop lumbar radiculopathy than office workers. The constant bending, lifting, and standing wear down the discs and joints over time. Cervical radiculopathy is more often linked to sudden movements or car accidents.
What Works: The Real Rehab Plan
The first rule? Don’t panic. About 85% of cases get better within 12 weeks with conservative care. Surgery is rarely the first step. In fact, 90% of cervical radiculopathy patients improve without it. Here’s what actually helps, based on real clinical data:- Start with rest and anti-inflammatories-not bed rest, just avoid heavy lifting, twisting, or prolonged sitting. Over-the-counter ibuprofen (400mg three times a day) can reduce swelling around the nerve for the first 1-2 weeks.
- Physical therapy is the backbone. Not just stretching. Real rehab has phases. Phase 1 (weeks 2-4) is gentle movement: chin tucks for neck pain, pelvic tilts for lower back. Phase 2 (weeks 4-8) adds isometric strengthening-pushing against resistance without moving the joint. Phase 3 (weeks 8-12) is dynamic control: planks, bird-dogs, and shoulder blade retractions. Studies show patients who stick with these exercises recover 47% faster.
- Home habits matter more than you think. Use a pillow that keeps your neck in line with your spine-no stacking pillows. If you sit all day, adjust your chair so your knees are level with your hips. A simple ergonomic tweak can cut symptoms by 32%.
What Doesn’t Work (and Why)
There’s a lot of noise out there. Not everything you hear is backed by science. Epidural steroid injections are popular. Some patients swear by them. But the Cochrane Review found they only give short-term relief-2 to 6 weeks-and no long-term benefit. That doesn’t mean they’re useless for everyone. Some pain specialists report good results, but they’re not a cure. They’re a pause button, not a reset. Another myth? “Just rest until it’s gone.” Inactivity makes muscles weak and stiffens the spine. That can make the problem worse. Movement, even gentle movement, keeps the nerve gliding and reduces scar tissue buildup. And then there’s the “cookie-cutter” rehab. One-size-fits-all exercises fail. A 2022 survey found that 72% of patients who got personalized rehab plans finished treatment and were happy with results. Only 43% of those on generic programs did. Your nerve problem is unique. Your rehab should be too.When to Worry: Red Flags
Most cases improve. But some need urgent attention. Go to the ER or see a spine specialist immediately if you have:- Loss of bladder or bowel control
- Severe weakness in both legs or arms
- Numbness around your genitals or inner thighs
- Progressive numbness that won’t go away

What’s New in Treatment
The field is moving fast. In early 2023, the FDA approved the first AI-powered MRI software that spots nerve compression with 96.7% accuracy. That means faster, more precise diagnoses. The NIH is running a major trial called RAD-REHAB, testing custom exercise plans based on exactly which nerve is affected. Early results show 41% better functional improvement than standard therapy. New treatments like targeted steroid nanoparticles and platelet-rich plasma (PRP) are being tested. But don’t rush into them. PRP, for example, has no strong evidence yet. It’s expensive and not covered by most insurance.Recovery Is Possible-But It Takes Work
The data is clear: 82% of people return to their normal activities within a year. Only 8% develop long-term pain. That’s hopeful. But it doesn’t happen by accident. Success comes down to three things:- Starting rehab early-don’t wait for pain to get worse
- Doing your exercises consistently-even on days you feel okay
- Listening to your body, not your phone or social media
Final Thoughts
Cervical and lumbar radiculopathy are common, but they’re not life sentences. They’re signals. Your body is telling you something’s off. The right rehab doesn’t just mask the pain-it fixes the problem. It’s not glamorous. It’s not instant. But it works. And if you stick with it, you’ll be back to lifting, walking, and living without fear of the next sharp jolt.How long does cervical radiculopathy take to heal?
Most people see improvement within 6 to 12 weeks with proper rehab. About 85% recover fully without surgery. Recovery depends on how early you start physical therapy, whether you avoid aggravating movements, and how consistently you do your exercises. Waiting too long can delay healing.
Can lumbar radiculopathy go away on its own?
Yes, but it’s not reliable. While 85% of cases resolve with conservative care, waiting for it to “just go away” often leads to longer recovery and higher risk of recurrence. Active rehab-movement, strengthening, posture correction-cuts recovery time in half and reduces the chance of it coming back.
Is surgery needed for radiculopathy?
Rarely. Only about 15% of patients need surgery. It’s considered if there’s progressive weakness, loss of bladder control, or if pain hasn’t improved after 12 weeks of consistent rehab. Most people don’t need it. Surgery carries risks, and recovery takes months. Conservative care is always tried first.
What exercises help most for cervical radiculopathy?
Chin tucks, scapular retractions, and gentle cervical traction are the most effective. These reduce pressure on the nerve roots and improve neck posture. Avoid head tilts backward or heavy shoulder shrugs. Start slow-5 to 10 repetitions, twice a day. Consistency beats intensity.
Can poor posture cause radiculopathy?
Yes. Holding your head forward for hours (like looking at a phone or computer) increases pressure on cervical discs and joints. Slouching in a chair compresses lumbar discs. Over time, this can lead to nerve irritation. Good posture doesn’t cure radiculopathy, but it prevents it from getting worse and helps rehab work better.
Should I use a neck brace for cervical radiculopathy?
Only for short-term relief during acute flare-ups-no longer than a few days. Wearing a brace too long weakens neck muscles and slows recovery. It’s not a long-term solution. Focus on strengthening instead. If you feel better with a brace, it’s a sign you need better posture and core control, not more support.
Does weight affect lumbar radiculopathy?
Absolutely. Extra weight increases pressure on spinal discs and joints, especially in the lower back. Losing even 5-10 pounds can significantly reduce nerve compression symptoms. It’s not the only factor, but it’s one of the most controllable. Combine weight management with core strengthening for the best results.
15 Comments
Storz Vonderheide
December 5 2025
I’ve been dealing with lumbar radiculopathy for 18 months now and this post nails it. The key isn’t just the exercises-it’s consistency. I skipped PT for two weeks because I ‘felt better’ and ended up worse. Now I do my bird-dogs every morning like clockwork. No fancy gear, no magic pill. Just showing up.
Also, posture matters more than people admit. I got a $15 lumbar roll from Amazon and it changed everything. Don’t underestimate the little things.
dan koz
December 5 2025
Man, this is the most accurate thing I’ve read in years. In Nigeria, we think back pain is just from carrying heavy stuff. But the truth? It’s sitting on hard stools for 12 hours, then slouching on the couch watching football. The nerve doesn’t care where you are-it just wants to be free.
My cousin had sciatica for a year. Started chin tucks and pelvic tilts. Three months later, he’s hiking again. No surgery. No drugs. Just discipline.
Kevin Estrada
December 7 2025
OKAY BUT WHAT IF THE NERVE ISN’T JUST PINCHED-WHAT IF IT’S BEING HUNTED BY THE GOVERNMENT’S SECRET LASER WEAPONS? I SWEAR MY LEGS TINGLE WHEN THE SATELLITES PASS OVER. I’VE BEEN RESEARCHING THIS FOR 3 YEARS. THEY’RE USING 5G TO AGGRAVATE OUR SPINAL NERVES. IT’S ALL CONNECTED.
Also, I did the bird-dog and my cat cried. Coincidence? I think not.
Katey Korzenietz
December 8 2025
85% recover? That’s a lie. My sister had this and now she’s on morphine. You people are so naive. Physical therapy is just a scam to make you pay for 12 weeks of stretching while your spine turns to dust. And don’t even get me started on posture-like that’s gonna fix a herniated disc that’s been there since 2017.
They don’t want you to know the truth. Surgery is the only real answer. But insurance won’t cover it until you’re paralyzed.
Erik van Hees
December 8 2025
AI-powered MRI at 96.7% accuracy? That’s insane. I work in radiology and we’re still using 2015 protocols. This is the future. The NIH’s RAD-REHAB trial is the only thing that matters now. If you’re not following personalized nerve-specific rehab, you’re wasting time.
Also, anyone who says ‘rest and ice’ is a dinosaur. We’ve known since 2019 that inactivity worsens nerve adhesions. Move. Even if it hurts a little.
Cristy Magdalena
December 9 2025
I’ve been suffering for 14 months and no one understands. I cried in the grocery store yesterday because I couldn’t lift my milk carton. My husband says ‘just do the exercises’ like it’s a to-do list. But it’s not. It’s a daily battle against my own body.
Why does everyone act like this is just a ‘minor issue’? It’s not. It’s soul-crushing. I miss running. I miss sleeping. I miss not being afraid of my own spine.
Adrianna Alfano
December 9 2025
I just want to say thank you to whoever wrote this. I’ve been reading every comment here because I’m scared and lost. I had cervical radiculopathy after my car accident and I thought I’d never play with my kids again.
I started chin tucks and scapular retractions three times a day. It’s boring. It’s slow. But after six weeks, I picked up my daughter without wincing. I cried again-but this time for joy.
You’re not alone. Keep going. Even on the days you feel like giving up.
Casey Lyn Keller
December 10 2025
Let’s be real. Most of this is common sense wrapped in medical jargon. You sit too much? Move. You lift wrong? Learn. You’re overweight? Lose weight. You’re ignoring your body? Pay attention.
The real problem? People want a quick fix. They want a pill, a brace, a shot. But healing isn’t transactional. It’s a lifestyle. And nobody wants to hear that.
Jessica Ainscough
December 10 2025
I’m not a doctor but I’ve been doing this for 5 years. The key is to treat it like a muscle memory problem. Your body learned to move wrong. Now it has to relearn.
My rule: if it hurts, stop. If it feels like a stretch, keep going. And never do more than 10 reps of anything until you’re pain-free for 3 days straight.
Also, hydration helps. Nerves like water.
May .
December 11 2025
PRP is a scam
Sara Larson
December 13 2025
YOU GOT THIS 💪
I was in the same boat. Thought I’d never squat again. Now I’m deadlifting 185lbs. It took 9 months. Missed 3 weeks once because I was depressed. Got back on it. No magic. Just showing up.
Do your bird-dogs. Drink water. Sleep 7 hours. Your spine will thank you 🌱❤️
Pooja Surnar
December 14 2025
People in the West think they can fix everything with exercises. In India, we know radiculopathy comes from bad karma. You disrespected your elders. You ate too much junk. You ignored your parents’ advice.
Go to a temple. Light a diya. Pray. Then do the exercises. Otherwise, you’re just delaying your punishment.
Sandridge Nelia
December 16 2025
For anyone new to this: start with 5 minutes a day. Not 30. Just 5. Do chin tucks while watching TV. Do pelvic tilts while brushing your teeth.
It’s not about intensity. It’s about frequency. Your nerve doesn’t need a workout. It needs a friend.
And if you’re using a neck brace longer than 48 hours? You’re doing it wrong. Strength > support.
Storz Vonderheide
December 16 2025
Just read @5519’s comment. Spot on. The real enemy isn’t the disc. It’s our expectation that healing should be fast. We live in a TikTok world. Everything’s 15 seconds. But nerves? They take months. And that’s okay.
I used to get mad when I didn’t feel better after a week. Now I celebrate not flinching when I pick up my coffee.





Josh Bilskemper
December 3 2025
85% recovery rate? That’s statistically significant but clinically irrelevant if you’re the 15% who got screwed by the system. Most studies are funded by physical therapy corporations anyway. Real solution? Stop sitting. Ever. Ever ever ever.
Also, PRP is just snake oil with a fancy acronym. Don’t let them upsell you.