Nerve Pain Relief: What Works, What Doesn’t, and How to Stay Safe
When you have nerve pain relief, treatment that targets damaged or overactive nerves, not just surface-level soreness. Also known as neuropathic pain, it doesn’t respond to regular painkillers like ibuprofen the way a sprained ankle does. This is the kind of pain that feels like burning, electric shocks, or pins and needles—often from diabetes, shingles, injury, or even long-term medication use. If you’ve tried OTC drugs and nothing helped, you’re not alone. Most people with nerve pain need something stronger—and that’s where things get tricky.
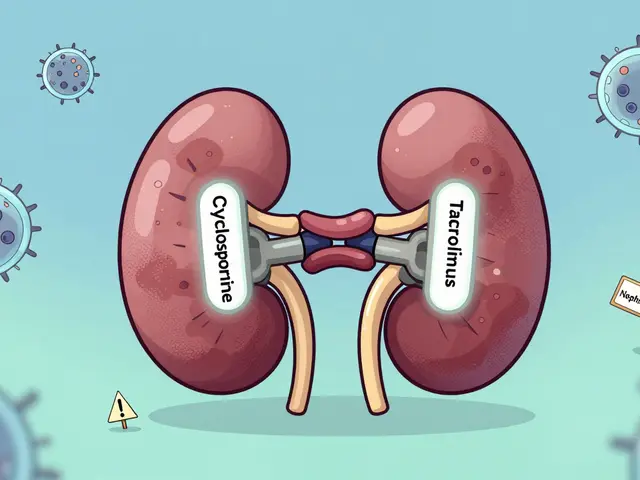
Prescription pain meds, drugs specifically designed to calm overactive nerve signals. Also known as anticonvulsants or antidepressants for pain, they’re not what you’d expect. Gabapentin, pregabalin, duloxetine—these aren’t painkillers in the traditional sense. They work by changing how nerves send signals to your brain. But here’s the catch: they can interact dangerously with other meds you’re taking. For example, mixing them with blood pressure drugs or sedatives can cause dizziness, falls, or even breathing problems. And if you’re on statins or antibiotics, you might not realize your nerve pain meds are making side effects worse. This isn’t just about finding something that works. It’s about finding something that works without putting you at risk.
Drug interactions, when two or more medications affect each other’s behavior in your body. Also known as adverse drug reactions, they’re one of the leading causes of hospital visits for people managing chronic pain. A study from the FDA found that over 40% of people taking nerve pain meds were also on at least one other drug that could clash with it. Grapefruit juice, certain antibiotics, even some herbal supplements can turn a safe dose into a dangerous one. That’s why checking labels before every pill matters—not just for safety, but because your nerve pain treatment might depend on timing, diet, or what else you’re taking.
And then there’s medication safety, the practice of using drugs correctly to avoid harm. Also known as medication adherence, it’s not just about taking your pills. It’s about knowing when to ask for help, how to track side effects, and when to push back if something feels off. Many people with nerve pain get stuck on meds that stop working—or cause new problems like weight gain, brain fog, or even liver damage. That’s why keeping a simple journal of what you take, when, and how you feel can make all the difference. You don’t need to be an expert. You just need to pay attention.
What you’ll find below isn’t a list of miracle cures. It’s a collection of real, practical advice from people who’ve been there—how to tell if your nerve pain meds are working, which ones to avoid with other conditions, and how to spot hidden risks before they become emergencies. These aren’t theory pages. They’re field guides for living with nerve pain without losing control of your health.
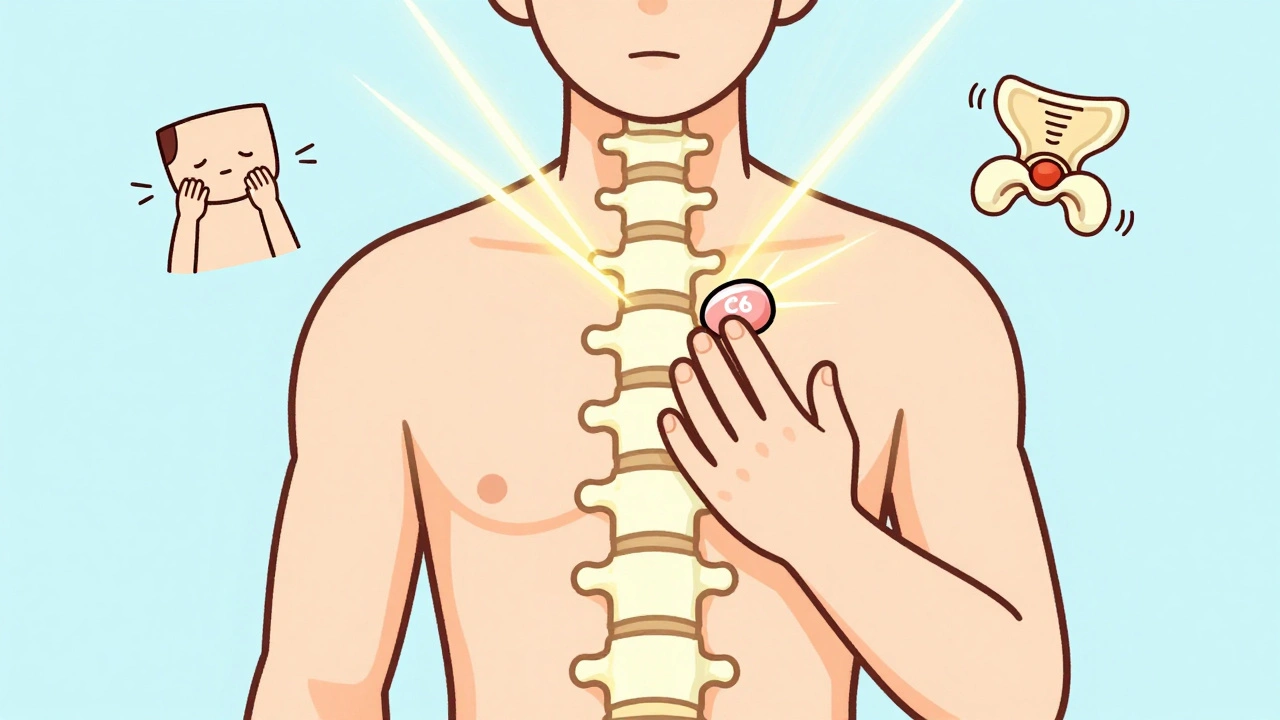
Cervical and Lumbar Radiculopathy: Nerve Pain and Rehabilitation That Actually Works
Cervical and lumbar radiculopathy cause nerve pain that shoots into arms or legs. Most cases improve with targeted rehab, not surgery. Learn what actually works, what doesn't, and how to recover faster.
View More