Calcineurin Inhibitor Side Effects Comparison
Cyclosporine vs Tacrolimus Side Effect Comparison
Compare the side effects of cyclosporine and tacrolimus based on clinical evidence. These drugs have similar mechanisms but different side effect profiles that can significantly impact quality of life.
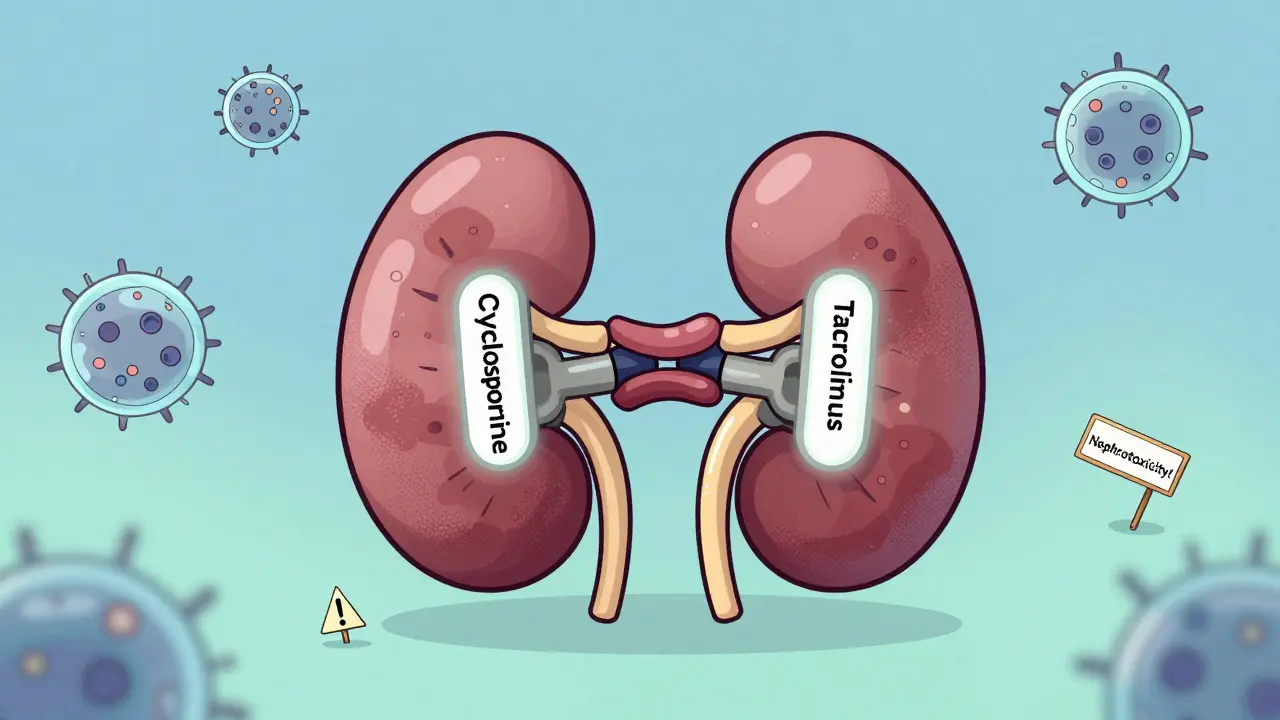
Nephrotoxicity
Neurotoxicity
Metabolic Side Effects
Other Side Effects
What You Should Do
If you're experiencing side effects from calcineurin inhibitors:
- Ask about your blood level monitoring schedule
- Track your symptoms in a journal
- Discuss dose reduction with your team
- Explore CNI-sparing protocols
- Consider alternatives like belatacept for low-risk patients
78% of patients would switch to a different drug if it worked as well with fewer side effects. Your quality of life matters as much as graft survival.
What Are Calcineurin Inhibitors?
Calcineurin inhibitors (CNIs) are powerful drugs used to stop your immune system from attacking a transplanted organ-or in some cases, from attacking your own body in autoimmune diseases. The two main ones are cyclosporine and tacrolimus. They work by blocking calcineurin, a protein that tells your T-cells to sound the alarm and launch an immune attack. Without that signal, your body is less likely to reject a kidney, liver, or heart transplant.
These drugs became standard in the 1980s and 1990s. Cyclosporine was the first, approved in 1983. Tacrolimus followed in 1994 and quickly became more popular because it worked better at preventing rejection. Today, about 85% of kidney transplant patients in the U.S. take tacrolimus, while only 10% still use cyclosporine. But even though tacrolimus is more effective, it comes with a heavier burden of side effects.
Most Common Side Effects: Nephrotoxicity
The biggest problem with both drugs is damage to the kidneys. This isn’t just a minor bump in lab results-it’s a real, measurable risk. About 25% to 75% of people on these drugs will see their creatinine levels rise, which means their kidneys aren’t filtering as well. This is called acute nephrotoxicity, and it’s often reversible if caught early.
But long-term use? That’s where things get serious. Around 10% to 30% of patients develop chronic kidney damage over years, with scarring in the tubules and tissue around them. A major study from 2009 found that calcineurin inhibitors were responsible for 38% of late kidney graft failures. That means nearly four in ten times a transplanted kidney fails after several years, it’s because of the very drug meant to save it.
Doctors manage this by keeping blood levels low-just enough to prevent rejection, but not so high that they wreck the kidneys. Trough levels for tacrolimus are usually kept between 5 and 10 ng/mL, and for cyclosporine, between 100 and 200 ng/mL. Monitoring happens weekly at first, then monthly once things stabilize.
Neurotoxicity: Tremors, Headaches, and Worse
Tacrolimus is far more likely than cyclosporine to cause neurological problems. Up to 70% of people on tacrolimus get hand tremors-sometimes so bad they can’t hold a cup or write their name. Cyclosporine causes tremors in only 10% to 25%. This isn’t just annoying; it can make driving, cooking, or even buttoning a shirt difficult.
Headaches, insomnia, and confusion are common. But the most alarming cases involve something called CNI-induced parkinsonism. A 2022 case report described a kidney transplant patient who developed shaking, slow movement, and stiffness just two weeks after starting tacrolimus. When they switched to cyclosporine, symptoms disappeared. But when they went back to cyclosporine months later, the tremors returned. That’s a red flag: even cyclosporine can trigger neurological issues in some people.
Some centers now do cognitive screening at three months for tacrolimus users. Up to 20% show subtle memory or attention problems. These aren’t always caught unless someone’s looking for them.
Metabolic Side Effects: Diabetes and High Blood Pressure
Tacrolimus is notorious for triggering new-onset diabetes after transplant. About 15% to 30% of people taking it develop diabetes, compared to 5% to 15% on cyclosporine. Why? It directly damages insulin-producing beta cells in the pancreas. This isn’t just about needing insulin shots-it raises the risk of heart disease, nerve damage, and kidney problems later on.
Doctors now recommend starting SGLT2 inhibitors like dapagliflozin at the first sign of high blood sugar. A 2021 trial showed this cut diabetes progression by 38% in tacrolimus users.
High blood pressure affects half to 70% of everyone on these drugs. It’s not just from fluid retention-it’s because CNIs narrow the blood vessels going into the kidneys. This forces the heart to work harder. Many patients need two or three blood pressure medications just to stay in range.
Other Key Differences: Hirsutism, Gum Swelling, and Stomach Issues
Cyclosporine has its own unique problems. About 20% to 30% of users grow more body hair-on their face, arms, back. It’s not just cosmetic; it affects self-esteem. About 15% to 25% get swollen, bleeding gums. Brushing teeth becomes painful. Dentists often see these patients for the first time because of gum overgrowth.
Tacrolimus, on the other hand, hits the gut harder. Nausea affects 30% to 45% of users, compared to 15% to 25% on cyclosporine. Diarrhea is even more common-25% to 40% versus 10% to 20%. Some patients lose weight because they can’t keep food down.
Both drugs cause low magnesium and high potassium. About half of patients need magnesium supplements to keep levels above 1.8 mg/dL. High potassium can be dangerous-it can cause heart rhythm problems. That’s why blood tests every few weeks are non-negotiable.
What Do Patients Really Experience?
Real-world data from transplant forums and surveys paint a clearer picture than clinical trials. On the American Transplant Foundation’s site, 68% of 1,245 patients said their side effects were moderate to severe. Tremors, sleep problems, and managing diabetes topped the list for tacrolimus users.
On Reddit’s r/transplant community, cyclosporine users complained about hirsutism in 42% of posts. Tacrolimus users mentioned tremors in 67%-nearly double the rate. One woman wrote: “I stopped hugging my kids because my hands shook so badly I was scared I’d drop them.”
Quality of life scores drop by 15 to 22 points on a 100-point scale when you’re on a CNI. That’s like going from feeling “okay” to feeling “badly unwell” every day. And here’s the kicker: 78% of patients surveyed by the National Kidney Foundation said they’d switch to a different drug if it worked just as well but had fewer side effects.
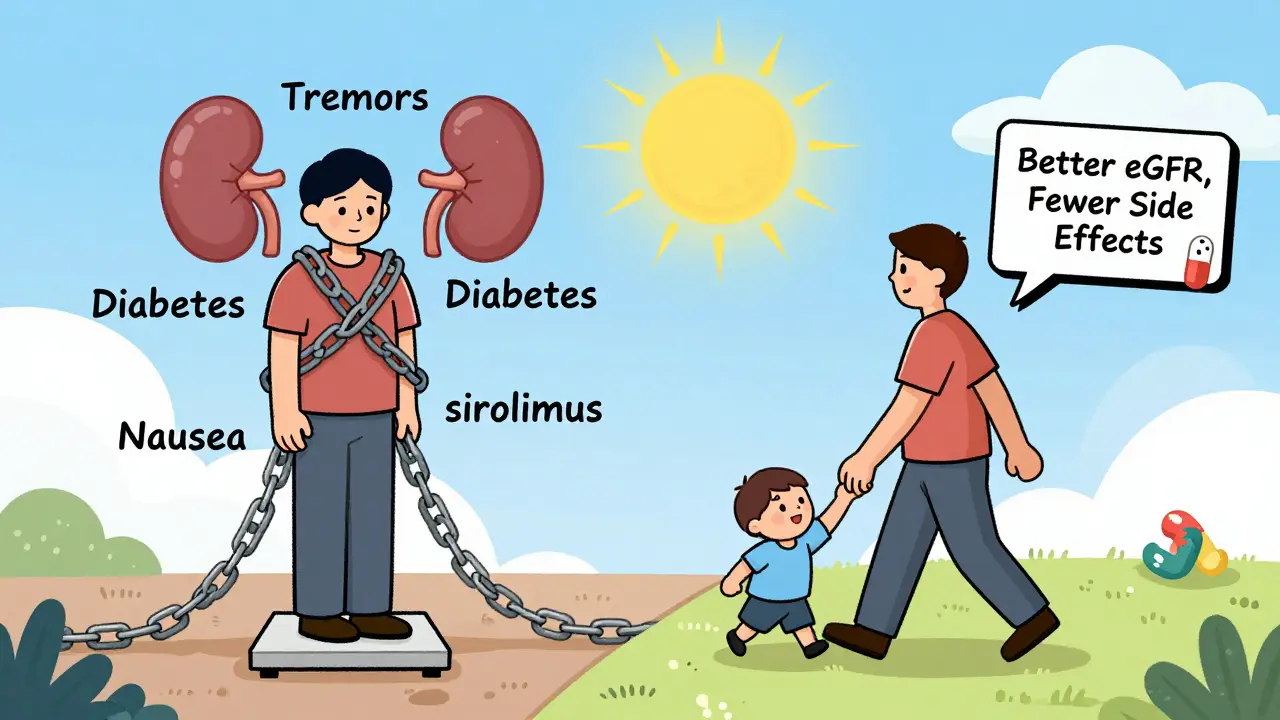
How Are Doctors Trying to Reduce These Side Effects?
The old approach was “more is better”-higher doses meant less rejection. Now, the goal is the opposite: minimum effective dose. Many centers now use CNI-sparing protocols, especially for low-risk patients. That means starting with a low dose of tacrolimus or cyclosporine and adding other drugs like mTOR inhibitors (everolimus, sirolimus) to boost protection without more toxicity.
Some patients are switched entirely off CNIs. Belatacept, a newer drug approved in the U.S., works without touching calcineurin. In a 2023 trial, patients on belatacept had better kidney function (eGFR 58.3 vs 49.1) and fewer metabolic issues than those on tacrolimus-with no difference in graft survival after three years.
Voclosporin, a newer CNI approved in 2021 for lupus nephritis, causes less high blood pressure than cyclosporine. It’s not yet used in transplants, but it shows what’s possible: a CNI with fewer side effects.
Trials are now testing whether early CNI withdrawal (within weeks of transplant) works for low-risk patients. Early results show 89% graft survival at one year-with 40% fewer side effects.
What Should You Do If You’re on One of These Drugs?
If you’re taking cyclosporine or tacrolimus, don’t stop. But do ask these questions:
- Is my blood level being checked regularly?
- Have my kidney function, blood sugar, and magnesium been tested in the last month?
- Are my tremors getting worse? Could my dose be lowered?
- Am I on the lowest dose that still prevents rejection?
- Has my doctor talked about switching to a CNI-free regimen?
Keep a symptom journal. Note when you feel shaky, tired, or nauseous. Bring it to your next appointment. Small changes-like lowering your dose by 0.5 mg or switching from tacrolimus to cyclosporine-can make a huge difference in quality of life.
And remember: you’re not alone. Thousands of transplant patients are managing these side effects every day. The goal isn’t just to survive-it’s to live well, with as few burdens as possible.
Are cyclosporine and tacrolimus the same thing?
No. Both are calcineurin inhibitors and work similarly to prevent organ rejection, but they’re chemically different. Tacrolimus is stronger and more effective at preventing rejection, but it also causes more side effects-especially tremors, diabetes, and stomach issues. Cyclosporine causes more hair growth and gum swelling. Doctors choose based on patient risk, tolerance, and side effect history.
Can you stop taking cyclosporine or tacrolimus?
Never stop without your transplant team’s guidance. Stopping suddenly can cause your body to reject the transplanted organ, which can be life-threatening. But many patients can safely reduce their dose or switch to a different drug over time-especially if they’re low-risk for rejection. This is called CNI minimization or withdrawal, and it’s now standard for about 30% of patients.
Which has more side effects: cyclosporine or tacrolimus?
Tacrolimus has a higher rate of neurotoxicity (tremors, headaches), new-onset diabetes, and gastrointestinal problems. Cyclosporine causes more cosmetic side effects like excessive hair growth and swollen gums. Both cause kidney damage, high blood pressure, and low magnesium. The choice often comes down to which side effects you can tolerate better.
Do calcineurin inhibitors cause permanent kidney damage?
They can. Acute kidney changes from CNIs are often reversible if caught early. But long-term use can lead to chronic interstitial fibrosis and tubular atrophy-scarring that doesn’t heal. Studies show this damage contributes to 38% of late kidney graft failures. Regular monitoring and dose adjustments can help reduce this risk.
Are there alternatives to cyclosporine and tacrolimus?
Yes. Belatacept is a CNI-free drug approved for kidney transplant patients that offers similar rejection protection with better kidney function and fewer metabolic side effects. mTOR inhibitors like sirolimus and everolimus are also used in CNI-sparing regimens. Newer drugs like voclosporin are being studied for broader use. The goal now is to minimize or eliminate CNIs when possible.
Final Thoughts: It’s Not Just About Survival
For decades, transplant medicine focused on one thing: keeping the organ alive. Today, the focus is shifting. It’s not enough to survive. You want to live. To sleep through the night. To hold your grandchild without shaking. To not need insulin because your pancreas still works.
Cyclosporine and tacrolimus saved millions of lives. But they came at a cost. Now, doctors are learning how to use them smarter-lower doses, earlier switches, better monitoring. And patients are speaking up. They’re demanding better quality of life, not just longer life.
If you’re on one of these drugs, you’re not just a patient. You’re a partner in your care. Ask questions. Track your symptoms. Push for alternatives if the side effects are too much. You’ve already done the hard part-getting the transplant. Now it’s time to make sure the rest of your life isn’t defined by the side effects of the drug that saved you.





Joseph Cooksey
February 3 2026
Let me tell you something nobody in the medical industry will admit out loud - these drugs aren’t just toxic, they’re a corporate gamble dressed up as science. Tacrolimus was pushed hard because it looked good on paper, but the real cost? Patients losing their dignity, their sleep, their ability to hold their own damn coffee cup. And don’t get me started on how the pharma reps hand out free pens while quietly watching your kidneys fail over time. I’ve seen it. I’ve lived it. It’s not ‘side effects’ - it’s systemic neglect wrapped in a white coat.
And yeah, belatacept sounds great on paper, but guess who pays the price when it fails? You. The system doesn’t care about your tremors or your insomnia - it cares about the next quarterly report. They’ll keep prescribing CNIs until someone sues them into oblivion. Until then, you’re just a data point with a transplanted organ and a broken spirit.
My cousin was on tacrolimus for five years. Lost 30 pounds from nausea, developed diabetes, and couldn’t hug her daughter without shaking like a leaf. They told her it was ‘normal.’ Normal? Normal is not having to cry in the bathroom because your own body betrayed you twice - once by needing a transplant, and again by the drug meant to save you.
Doctors act like they’re saving lives, but they’re just delaying the inevitable. They don’t have the courage to say, ‘Hey, maybe we should try something else before you’re on insulin and dialysis at 42.’ And guess what? You’re supposed to be grateful. Grateful for being alive. But alive isn’t the same as living.
There’s a whole generation of transplant patients who can’t sleep, can’t work, can’t enjoy a meal without fearing their next blood test. And the system? It just keeps handing out more pills. More labs. More ‘adjustments.’
It’s not medicine anymore. It’s a slow-motion hostage situation - and the ransom is your quality of life.