When you take a new medication and feel unwell, it’s natural to worry: is this a drug allergy, or just a side effect? The answer matters more than you think. Mislabeling a side effect as an allergy can lead to worse health outcomes, higher costs, and even life-threatening choices - like being given a stronger antibiotic that increases your risk of C. diff infection. On the flip side, ignoring a real allergy could mean anaphylaxis. The difference isn’t just medical jargon - it’s about your safety.
What Is a True Drug Allergy?
A true drug allergy happens when your immune system mistakes a medication for a threat - like a virus or pollen - and attacks it. This isn’t just feeling sick. It’s your body activating antibodies, releasing histamine, and triggering inflammation. The most common triggers? Penicillin and other beta-lactam antibiotics. About 80% of all documented drug allergies involve these drugs.There are two main types of allergic reactions:
- Immediate (IgE-mediated): Happens within minutes to an hour after taking the drug. Symptoms include hives, swelling of the face or throat, wheezing, vomiting, and in severe cases, anaphylaxis - a drop in blood pressure and trouble breathing that can be fatal.
- Delayed (T-cell mediated): Shows up days or even weeks later. Think rash, fever, swollen lymph nodes, or organ inflammation. One serious form is DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms), which can damage your liver, kidneys, or lungs and has a 10% death rate if not caught early.
Here’s the key: a true allergy means your body remembers the drug. If you take it again, even years later, the same reaction can happen - sometimes worse. That’s why doctors treat these reactions seriously.
What Are Side Effects?
Side effects are predictable, non-immune reactions caused by how a drug works in your body. They’re listed in the patient information leaflet for a reason - they’re common, known, and usually not dangerous. Think of them like the unintended side of a tool’s main function.Examples:
- Statins causing muscle aches - because they interfere with cholesterol production in muscle cells.
- ACE inhibitors causing a dry cough - due to buildup of bradykinin, a chemical that irritates the throat.
- Metformin causing diarrhea - because it changes gut bacteria and draws water into the intestines.
- SGLT2 inhibitors (like dapagliflozin) increasing urination - because they make your kidneys flush out sugar.
These reactions don’t involve your immune system. They’re dose-dependent, meaning higher doses usually make them worse. And often, they fade over time as your body adjusts. Many people stop their meds because they think it’s an allergy - but it’s just a side effect.
Timing Tells the Story
One of the best ways to tell the difference? When the reaction happens.If you took amoxicillin for a sore throat and broke out in hives 30 minutes later - that’s likely an allergy. If you started the same antibiotic and got nausea on day two, but it got better by day five? That’s a side effect. If you developed a full-body rash two weeks after starting allopurinol? That could be DRESS - a delayed allergic reaction.
Penicillin allergies? In 80-90% of cases, symptoms show up within an hour. But side effects from antibiotics like nausea, diarrhea, or yeast infections? They usually start within the first 72 hours and don’t get worse with each dose. In fact, they often improve as your body adapts.
Why Mislabeling Costs Lives - and Money
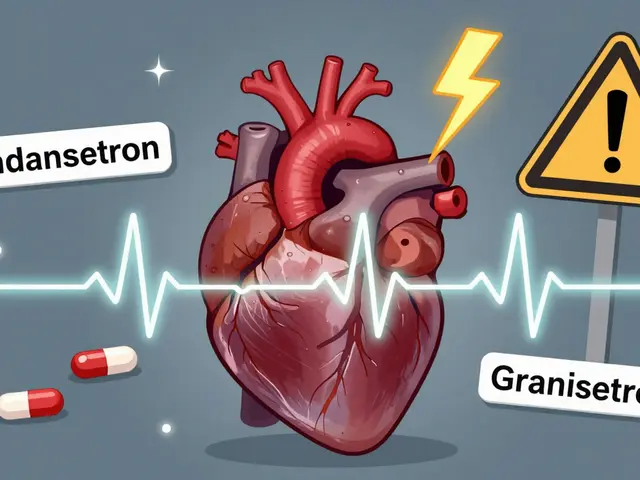
Here’s the scary part: up to 95% of people who say they’re allergic to penicillin aren’t. They had a rash as a kid, or got sick after taking the drug, and were told, “You’re allergic.” But when tested, most can take it safely.Why does this matter?
- Patients labeled as penicillin-allergic are 69% more likely to get broad-spectrum antibiotics like vancomycin or clindamycin - drugs that kill good bacteria and raise your risk of deadly C. diff infections.
- Each hospital stay for someone with a mislabeled penicillin allergy costs about $1,025 more than for someone who can take the right drug.
- In the U.S. alone, this mislabeling adds up to over $1 billion a year in extra healthcare costs.
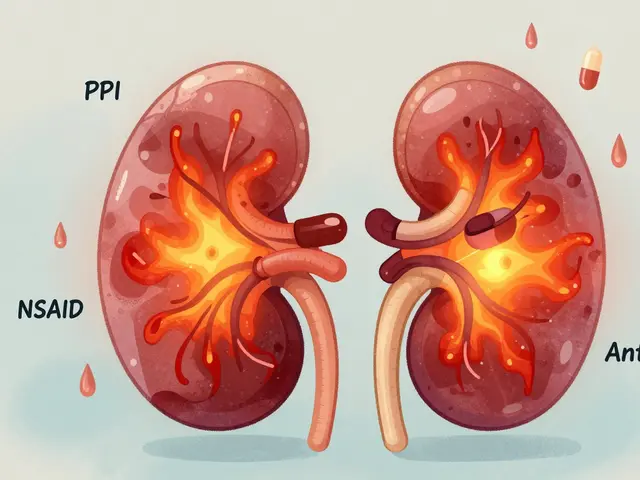
And it’s not just penicillin. People avoid sulfa drugs, NSAIDs, or even aspirin because they had a headache or stomach upset - but those aren’t allergies. They’re side effects. Avoiding effective treatments means more pain, longer illness, and more trips to the ER.

How to Know for Sure - Testing and Diagnosis
If you think you have a drug allergy, don’t assume. Don’t just rely on what a doctor said 20 years ago. Ask for a proper evaluation.For penicillin, the gold standard is skin testing - a tiny prick or injection of the drug under the skin. If there’s no reaction, you’re likely not allergic. Then, a supervised oral challenge (taking a small dose under watch) confirms it. This process has a 97-99% accuracy rate for ruling out true allergy.
For delayed reactions like rashes, doctors look for signs like:
- Eosinophils (a type of white blood cell) above 500 cells/μL in blood tests
- Atypical lymphocytes
- Organ involvement (liver enzymes up, kidney function down)
These help confirm DRESS or other immune-mediated reactions. For other drugs, there’s no easy test - but a detailed history, timing, and symptoms can point to the right diagnosis.
What You Can Do Right Now
You don’t need to wait for a specialist to start making smarter choices.- Write down your reaction: Not just “allergic to penicillin.” Write: “Got hives 20 minutes after taking amoxicillin. Swelling in lips. Needed epinephrine.” That’s a true allergy. Or: “Felt nauseous after starting metformin. Improved after a week.” That’s a side effect.
- Ask your doctor: “Was this an allergy or a side effect? Can we test it?”
- Check your records: If your EHR just says “Penicillin Allergy,” ask for a review. Many hospitals now have pharmacist-led allergy clinics that re-evaluate labels.
- Don’t avoid meds based on fear: If you were told you’re allergic to sulfa because you got a rash with Bactrim - but you’ve taken other sulfa drugs without issue? That’s not an allergy. That’s a coincidence.
Pharmacist-led programs have cut inappropriate penicillin avoidance by 80% in the VA system. You don’t need to be in a big hospital to benefit - ask your local pharmacy if they offer allergy reviews.
Real Stories, Real Consequences
One patient in Bristol told me she avoided all antibiotics for 15 years because she got a rash as a child while on amoxicillin. Turns out, she had roseola - a viral infection - at the time. The rash was from the virus, not the drug. When she finally got tested, she could safely take penicillin. Her UTIs? Treated in days, not weeks.Another man avoided ibuprofen for years because he thought it gave him “allergic hives.” He had kidney pain after taking it while dehydrated. Turns out, it was acute kidney injury - not an allergy. Once he understood, he could take it safely if he stayed hydrated.
And then there’s the woman who refused statins because of muscle pain. Her doctor explained: “This is a known side effect. We can lower the dose, switch types, or add CoQ10. It’s not an allergy.” She stayed on her statin, avoided a heart attack, and now feels better than ever.

The Bigger Picture
This isn’t just about one drug. It’s about how we use medicine safely. The FDA now requires drug labels to clearly separate allergy warnings from side effect lists. Hospitals are training staff to ask better questions. And research is underway to find blood biomarkers that can instantly tell if a reaction is immune-driven or just a pharmacological quirk.By 2027, most U.S. hospitals will have EHR alerts that pop up when a doctor prescribes a broad-spectrum antibiotic to someone labeled “penicillin-allergic” - asking, “Have you been tested?” That’s progress.
But it starts with you. If you’ve ever said, “I’m allergic to this,” ask yourself: What actually happened? Was it a rash? Nausea? Dizziness? When? Did you need emergency treatment? Or did it just make you feel off for a few days?
That detail - that truth - could save your life. Or at least, save you from taking a drug that’s less effective, more expensive, and riskier than the one you’re avoiding.
When to See an Allergist
You don’t need to see one for every little reaction. But if any of these apply, make an appointment:- You had swelling of the face, lips, or tongue
- You had trouble breathing or felt like you were going to pass out
- You had a rash that spread quickly and was accompanied by fever or blistering
- You’ve been told you’re allergic to more than one drug
- You’ve avoided a drug for years but never had a formal test
Most allergy clinics offer skin testing and oral challenges - and they’re covered by insurance. The goal isn’t to scare you. It’s to give you back the right options.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy as a child lose it within 10 years - even without testing. But unless you get tested, you won’t know for sure. Many adults carry a label they don’t need, just because they never re-evaluated it.
If I had a reaction once, will I always react?
For true allergies - yes. Your immune system remembers. But if the reaction was a side effect, like nausea or dizziness, you may not have it again. Side effects often fade with time or dose changes. The key is knowing which one you had.
Can a side effect become an allergy?
No. A side effect is a direct chemical reaction - not immune-based. But sometimes, a side effect can mask or trigger a real allergy. For example, if you got a rash from a viral infection while taking amoxicillin, your doctor might wrongly call it an allergy. Later, if you take penicillin again and get a true allergic reaction, it looks like you “developed” the allergy - but you didn’t. You just had a coincidence the first time.
Are over-the-counter drugs like ibuprofen or acetaminophen common causes of allergies?
True allergies to NSAIDs like ibuprofen are rare - under 1% of users. Most people who say they’re allergic actually have side effects like stomach upset or headaches. A true NSAID allergy usually causes hives, swelling, or breathing problems - not just nausea. Acetaminophen allergies are even rarer. If you’ve had a reaction, document the symptoms and timing before avoiding it long-term.
What should I do if I’m told I’m allergic but feel fine taking the drug?
Don’t stop - but don’t assume it’s safe either. Ask your doctor: “Was this reaction tested? Can we confirm it’s not an allergy?” Many people take drugs they think they’re allergic to, and nothing happens - but that doesn’t mean it’s safe. Only a proper evaluation can tell you for sure. If you’ve never been tested, consider it. It’s not risky, and it could open up better treatment options.
Final Thought: Know Your Reaction, Not Just the Label
You don’t need to be a doctor to understand the difference. You just need to pay attention. Write down what happened. When? How bad? Did you need emergency care? Did it go away on its own? That’s the real power - knowing your body’s response, not just accepting a label from years ago.Medications are tools. Like any tool, they have side effects. But only a few are dangerous because your immune system attacks them. Don’t let fear stop you from the right treatment. Get the facts. Ask the questions. And if you’ve been told you’re allergic - make sure it’s true.
14 Comments
Nishant Garg
January 18 2026
Man, this is one of those posts that makes you feel like you’ve been living in a fog your whole life. I remember my mom getting labeled ‘allergic to penicillin’ after a rash at age 7 - turns out she had chickenpox. She spent 30 years on clindamycin, got C. diff twice, and never knew she could’ve had the right drug. This isn’t just medical info - it’s a cultural blind spot. We treat labels like tattoos, when they’re more like sticky notes that should be updated every decade.
Also, why do we let doctors write ‘penicillin allergy’ in charts like it’s gospel? If your EHR says ‘allergy’ and you’ve never been tested, that’s not a diagnosis - it’s a ghost story.
Nicholas Urmaza
January 19 2026
This is exactly the kind of info that saves lives but gets buried under paperwork. Stop letting people self-diagnose allergies based on nausea or a rash. If you didn’t get an EpiPen and a trip to the ER you weren’t allergic. Period. Hospitals need to start auto-flagging these labels and forcing re-evaluation. This isn’t optional - it’s a public health crisis.
And yes I’m mad about it.
Sarah Mailloux
January 20 2026
I had no idea so many people are mislabeled. My sister thought she was allergic to ibuprofen because she got a headache once - turns out she was dehydrated. She’s been in pain for years avoiding it. This post should be mandatory reading for every high school health class.
Also - thank you for not using medical jargon. I actually understood it.
Nilesh Khedekar
January 21 2026
Ohhh so THAT’S why my grandma’s ‘penicillin allergy’ kept her on expensive antibiotics for 20 years? And now she’s got kidney damage from vancomycin? Classic. I mean, come on. We label people like they’re gluten-free at a buffet. ‘Oh you felt weird once? You’re allergic!’
Meanwhile, the system just keeps prescribing the wrong stuff and billing insurance. Someone’s making bank off our ignorance.
Also - why do pharmacists still stamp ‘ALLERGY’ on your file like it’s a death sentence? Who approved this medieval practice?
Jami Reynolds
January 22 2026
Let’s be real - this whole ‘drug allergy’ narrative is a distraction. The real issue? Pharma companies pushed antibiotics like candy for decades. They didn’t care if people got rashes - they made money. Now they’re selling ‘allergy testing’ as a new revenue stream. The FDA? Complicit. The EHR alerts? A PR stunt. They don’t want you to know the truth: most ‘allergies’ are just side effects, and the system profits from keeping you scared and on expensive drugs.
And don’t get me started on how they’ve been hiding the real causes of DRESS for years.
It’s not about your body - it’s about corporate control.
RUTH DE OLIVEIRA ALVES
January 23 2026
It is imperative to underscore the clinical significance of differentiating between immune-mediated drug hypersensitivity reactions and non-immune-mediated pharmacological side effects. The former necessitates lifelong avoidance and carries substantial morbidity and mortality risk; the latter, often transient and dose-dependent, may be mitigated through pharmacokinetic or pharmacodynamic adjustment.
Furthermore, the misclassification of non-allergic adverse events as true allergies contributes significantly to antimicrobial stewardship challenges, increased healthcare expenditures, and suboptimal therapeutic outcomes. The data presented herein are robust and align with current guidelines from the American Academy of Allergy, Asthma & Immunology (AAAAI) and the Joint Task Force on Practice Parameters.
It is therefore strongly recommended that all patients with a documented drug allergy undergo formal evaluation by a board-certified allergist-immunologist, particularly in cases involving beta-lactam antibiotics, where skin testing demonstrates greater than 95% negative predictive value.
Crystel Ann
January 23 2026
I had a rash after taking amoxicillin when I was 8. My mom said I was allergic. I avoided all antibiotics for 15 years. Then I got a UTI and my doctor said, ‘Let’s test it.’ Turned out I was fine. I cried in the clinic. Not because I was scared - because I realized I’d been scared for nothing.
Thank you for writing this. I needed to see someone say it out loud.
Jan Hess
January 24 2026
Biggest takeaway? Don’t let a 10-year-old diagnosis dictate your health for life.
My uncle thought he was allergic to sulfa because he got a stomachache once. Turns out he was sick with the flu. He avoided all antibiotics for 30 years. Last year he got sepsis from a simple infection because he refused to take the right drug.
We need to stop treating medical labels like family heirlooms. Time to update them.
Iona Jane
January 25 2026
So let me get this straight - the government lets hospitals keep ‘allergy’ labels that are 95% wrong… and they don’t even have to prove it?
And now they’re going to add ‘alerts’? Like that’s going to fix anything? I bet the real reason they’re doing this is because they’re getting sued for C. diff deaths.
They’re not trying to help us - they’re trying to cover their asses.
And don’t tell me ‘it’s for safety’ - if it was, they’d test everyone before prescribing. But they don’t. Because testing costs money.
They’d rather keep you sick than lose a profit margin.
Jaspreet Kaur Chana
January 26 2026
Bro this is wild. In India, we just get a scrip and go - no one asks, ‘When did it happen? What did it feel like?’ My cousin got labeled ‘penicillin allergic’ after a fever rash at 5. Now she’s on azithromycin for every sniffle. She’s got yeast infections every month. Her mom says ‘it’s better than risking death.’ But what if she’s not at risk? What if she’s just been living with side effects she doesn’t even know are avoidable?
We need to start asking questions. Not just taking what the doctor says as law. Especially when the doctor’s in a hurry and you’re just a number.
Haley Graves
January 26 2026
If you’ve ever been told you’re allergic to a drug and never tested - you owe it to yourself to get it checked. Not because it’s trendy. Not because some Reddit post said so. Because your life might depend on it.
And if your doctor brushes you off? Find a new one. This isn’t optional. It’s basic healthcare hygiene.
Diane Hendriks
January 28 2026
This is what happens when you let the weak-minded dictate medical policy. You have people who can’t tell the difference between a stomach ache and anaphylaxis - and they’re allowed to carry labels that alter their entire medical trajectory. Meanwhile, the elite know the truth: real allergies are rare. The rest? Weak constitutions and poor self-diagnosis.
The solution? Stop coddling. Start testing. And if you can’t handle a little nausea? Maybe you shouldn’t be on medicine at all.
This country is falling apart because we’ve turned health into a popularity contest.
ellen adamina
January 29 2026
Wait - so if I had a rash after taking penicillin as a kid, but it was during a viral infection… and I’ve taken it again since and been fine… does that mean I was never allergic?
And if so… why did my doctor never tell me to get tested?
I think I need to call my pharmacy tomorrow.




Ayush Pareek
January 16 2026
Really appreciate this breakdown. I used to panic every time I got a stomachache after antibiotics, but now I know it’s probably just a side effect. Took me years to figure that out.
Thanks for making it so clear.