Substance Use Disorder: Causes, Treatments, and What Really Works
When someone struggles with substance use disorder, a chronic condition where compulsive drug or alcohol use harms health, relationships, and daily function. Also known as addiction, it’s not a moral failure—it’s a brain disease that changes how reward, motivation, and self-control work. Many people think quitting is just a matter of willpower, but the truth is more complex. Brain chemistry shifts over time, making cravings feel impossible to ignore. That’s why treatment needs to go beyond willpower—it needs science, support, and the right meds.
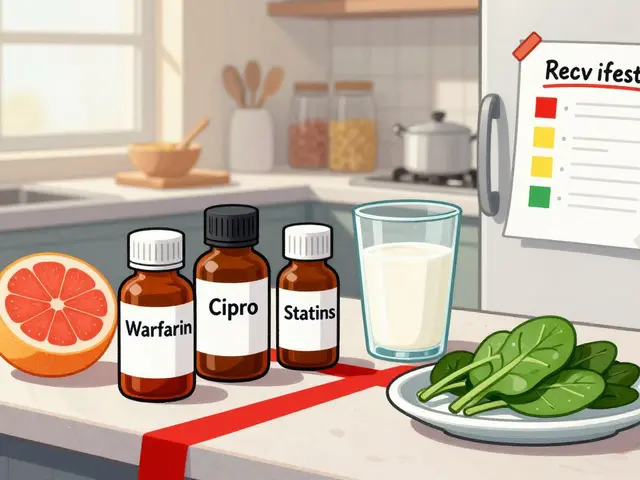
Medications like bupropion, an antidepressant that reduces cravings and withdrawal symptoms without causing sexual side effects common in other drugs are used off-label for smoking cessation and sometimes for alcohol or stimulant use. Meanwhile, SSRIs, a class of antidepressants that boost serotonin to ease anxiety and depression often linked to addiction help when mood disorders fuel substance use. But here’s the catch: these drugs don’t work the same for everyone. Bupropion might spark anxiety in some, while SSRIs can lower libido or cause weight gain—side effects that make people quit. And when you mix them with other meds, like blood pressure drugs or painkillers, risks go up fast. Drug interactions aren’t just a footnote—they’re a major reason treatment fails.
What’s missing from most conversations is how personal this journey is. One person finds freedom with therapy and bupropion. Another needs a medication journal to track how generics affect them. Someone else finds relief with prazosin for PTSD-triggered drinking. There’s no universal fix, but there are proven paths. The posts below dive into exactly that: real-world comparisons of meds, how to avoid dangerous combos, how to track your own response, and what works when standard treatments fall short. You’ll find no fluff—just clear, practical info from people who’ve been there.

How to Talk to Your Doctor About Overdose Risk Without Being Judged
Learn how to talk to your doctor about overdose risk using clear, evidence-based language that reduces stigma and increases your chances of getting life-saving help like naloxone.
View More