Rheumatology: Understanding Joint Pain, Autoimmune Diseases, and Treatment Options
When your joints ache for no clear reason, or your hands swell up in the morning, you might be dealing with something deeper than just aging. That’s where rheumatology, the branch of medicine focused on autoimmune and inflammatory conditions affecting joints, muscles, and connective tissues. Also known as rheumatic medicine, it deals with conditions that don’t show up on X-rays right away but can wreck your life if ignored. This isn’t just about arthritis—it’s about your immune system turning on your own body, and the doctors who figure out why.
Rheumatology includes arthritis, a group of over 100 conditions causing joint inflammation, pain, and stiffness, from common osteoarthritis to aggressive forms like rheumatoid arthritis. It also covers autoimmune diseases, where the body attacks its own tissues, often triggering systemic symptoms like fatigue, fever, and organ damage. Conditions like lupus, psoriatic arthritis, and vasculitis fall under this umbrella. These aren’t rare outliers—they affect millions, and many go undiagnosed for years because symptoms start slow and look like other things. That’s why knowing the red flags matters: morning stiffness lasting more than 30 minutes, unexplained fatigue, rashes that appear with joint pain, or swelling in fingers and toes without injury.
What you’ll find in this collection isn’t just textbook definitions. These posts connect rheumatology to real-world problems: how certain drugs can trigger joint pain, how generic meds for autoimmune conditions might behave differently in your body, and how lifestyle choices—like exercise, diet, and even medication timing—can make or break your daily function. You’ll see how drug interactions with common pain relievers can worsen inflammation, how monitoring blood levels helps avoid toxicity in long-term treatments, and why some people respond better to one therapy over another. This isn’t theory. It’s what happens when someone with rheumatoid arthritis switches generics and feels worse, or when a patient on a beta-blocker for high blood pressure can’t walk without exhaustion because their meds are masking symptoms they didn’t know were connected.
There’s no one-size-fits-all fix in rheumatology. What works for one person’s joint pain might do nothing—or make things worse—for another. That’s why tracking your response, understanding your meds, and knowing when to push back on a doctor’s advice isn’t being difficult—it’s essential. The posts here give you the tools to ask better questions, spot hidden risks, and take control without waiting for a specialist to solve everything for you.
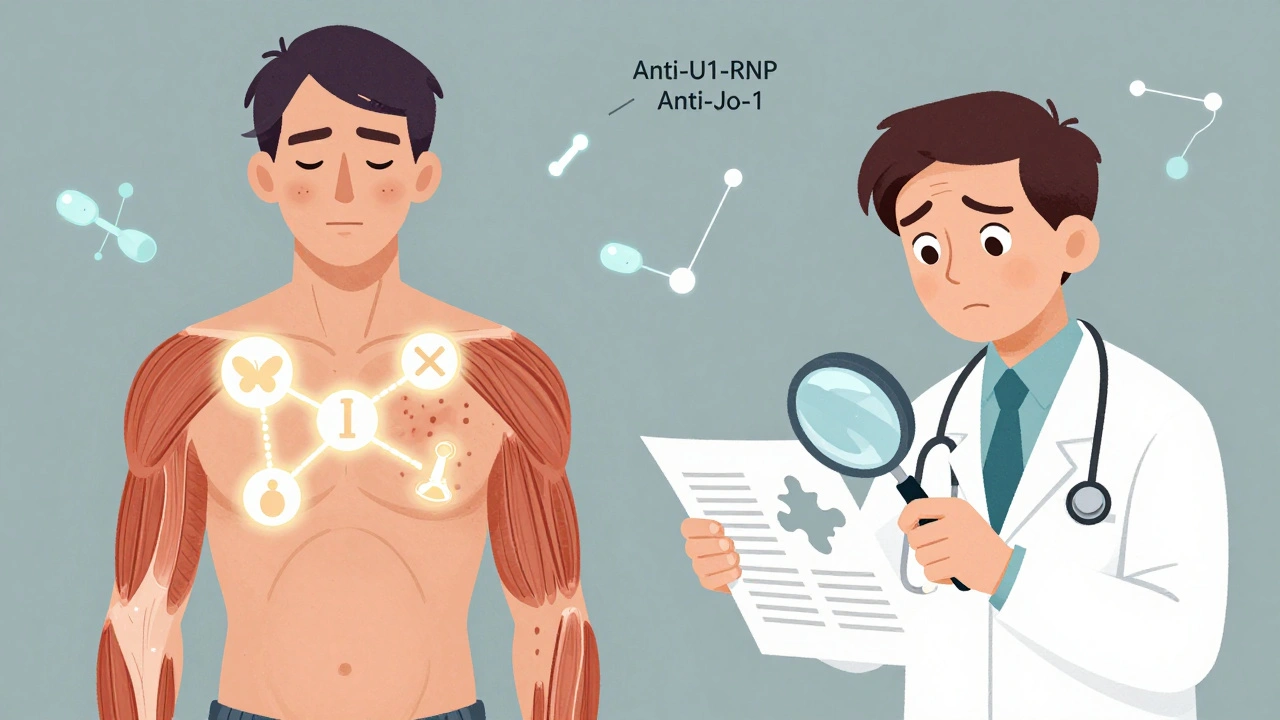
Autoimmune Overlap Syndromes: Recognizing Mixed Features and Coordinating Care
Autoimmune overlap syndromes occur when patients show features of multiple autoimmune diseases at once, like lupus, scleroderma, and myositis. Diagnosis is challenging, but specific antibodies and coordinated care can improve outcomes.
View More