
If you’ve been coughing up mucus for months - or years - and it won’t go away, you’re not just dealing with a stubborn cold. You might have chronic bronchitis. It’s not something you shake off after a week. It’s a long-term condition that changes how your lungs work, and it’s often tied to one thing: smoking. But here’s the good news: even if you’ve smoked for decades, quitting now can still make a huge difference. Not just in how you feel day to day, but in how long you’ll live.
What Chronic Bronchitis Really Means
Chronic bronchitis isn’t just a bad cough. It’s a clinical diagnosis: a productive cough that lasts at least three months in each of two consecutive years, along with airflow blockage in the lungs. That mucus? It’s your body’s attempt to protect itself from irritation - but too much of it clogs your airways, making it harder to breathe. It’s one of the two main forms of COPD (chronic obstructive pulmonary disease), the fourth leading cause of death in the U.S.By age 65, about 1 in 10 adults has some level of chronic bronchitis. Most of them - 75% - are current or former smokers. But it’s not just smokers. Long-term exposure to fumes, dust, or air pollution can trigger it too. And in rare cases, a genetic condition called alpha-1 antitrypsin deficiency plays a role. The damage to your airways doesn’t reverse, but it doesn’t have to keep getting worse.
The Symptoms You Can’t Ignore
You might think it’s just a smoker’s cough. But chronic bronchitis brings more than just noise. Here’s what most people experience:- A daily cough that won’t quit - often worse in the morning
- Thick mucus you have to clear several times a day
- Shortness of breath during simple tasks like walking to the mailbox or climbing stairs
- Chest tightness or pressure
- Wheezing - a whistling sound when you breathe
- Constant fatigue, even after resting
These aren’t minor annoyances. In fact, 82% of people with chronic bronchitis say breathing becomes hard during physical activity. And 68% report chest discomfort. If you’re avoiding walks, skipping chores, or feeling winded just talking, it’s not normal aging. It’s your lungs signaling they need help.
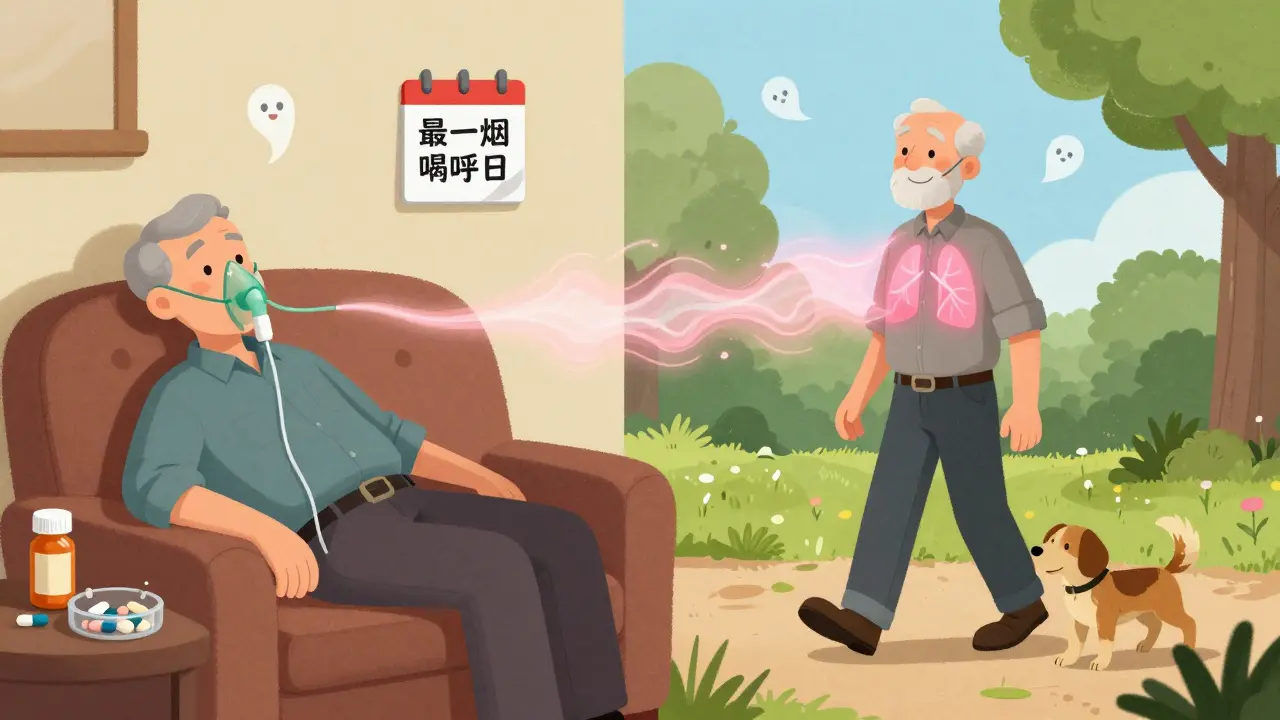
Why Smoking Cessation Is the Only Real Cure
There’s no pill that cures chronic bronchitis. No surgery. No miracle spray. But there is one intervention that changes everything: quitting smoking.Studies show that people who quit after being diagnosed slow the decline in lung function by 60% compared to those who keep smoking. That’s not a small gain - it’s life-altering. One 30-year study found that 42% of current smokers developed chronic bronchitis. Among former smokers? Just 26%. Even if you’ve smoked for 40 years, quitting at 60 still adds years to your life.
And it’s not just about stopping cigarettes. It’s about removing all lung irritants. Avoid secondhand smoke. Stay indoors on high-pollution days. Skip wood-burning stoves and strong cleaning fumes. Your lungs are already damaged - they don’t need more punishment.

What Works to Manage Symptoms - and What Doesn’t
Once you’ve quit, treatment focuses on keeping symptoms under control and preventing flare-ups. Not every treatment works for everyone, and some have serious downsides.What helps:
- Bronchodilators - inhalers that open your airways. Short-acting ones work in 15 minutes and last 4-6 hours. Long-acting ones are for daily use. They’re the first-line treatment for most patients.
- Pulmonary rehabilitation - this isn’t just exercise. It’s a full program: breathing techniques, nutrition advice, education, and supervised physical training. People who complete it walk 78 meters farther in six minutes and are 37% less likely to end up in the hospital.
- Vaccines - get the flu shot every year. It cuts your risk of a bad flare-up by 42%. Also get the pneumococcal vaccine every 5-7 years. It reduces pneumonia risk by 68%.
- Mucolytics - drugs like N-acetylcysteine help thin mucus so you can cough it up easier. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends them for regular use. They reduce flare-ups by about one every three years.
What to be careful with:
- Inhaled steroids - they reduce inflammation but increase your risk of osteoporosis by 23%, high blood pressure by 18%, and diabetes by 15% over time. Only use them if your doctor says you really need them.
- Antibiotics - they’re only helpful during bacterial infections, not for daily cough. Overuse leads to resistance. Amoxicillin-clavulanate works well when you have an infection, but don’t take them “just in case.”
- Over-the-counter cough suppressants - they’re often useless and can make things worse by trapping mucus in your lungs.
Getting Support to Quit Smoking
Quitting isn’t just willpower. It’s a medical process. And most people need help.People who try to quit on their own have a 7% success rate. Those who use professional support - like counseling, nicotine patches, gum, or prescription meds like varenicline - hit 45% success at six months. That’s a six-fold increase.
Combine quitting with pulmonary rehab, and your odds jump even higher. One study showed 52% of people stayed smoke-free after a year when they got both. That’s more than double the success of quitting alone.
Here’s what works in real life:
- Call a quitline - free, confidential, and staffed by counselors who’ve helped thousands.
- Use nicotine replacement - patches, gum, or lozenges - for at least 12 weeks.
- Ask your doctor about varenicline or bupropion - they reduce cravings and withdrawal.
- Join a support group - online or in person. Sharing struggles makes them easier to handle.
One patient, a 58-year-old man from Bristol, told his doctor he’d been coughing so badly he couldn’t sleep. After six months of rehab and quitting smoking, he walked to the end of his street without stopping - something he hadn’t done in three years.
What to Expect When You Start Treatment
You won’t feel better overnight. But you will feel progress - if you stick with it.Within weeks of quitting, your lungs start clearing mucus. Your cough may get worse at first - that’s your lungs cleaning out years of buildup. It’s temporary. After three months, breathing usually improves. By six months, many people notice they’re less tired and can walk farther.
Pulmonary rehab takes time, too. Most programs run 6-12 weeks, twice a week. You’ll learn how to breathe more efficiently, how to pace yourself, and how to recognize when you’re pushing too hard. It’s not easy, but 78% of people who finish say their daily life improved dramatically.
Medication adherence is a real challenge. Nearly half of patients don’t take their inhalers correctly. Some forget. Others can’t coordinate the puff with the breath. That’s why working with a respiratory therapist matters. On average, it takes 4-5 sessions to get it right.
When Oxygen and Other Advanced Treatments Come In
If your blood oxygen drops below 88%, your doctor may recommend long-term oxygen therapy. It’s not a last resort - it’s a life-extending tool. For people with severe disease, using oxygen 15+ hours a day increases five-year survival by 21%.New treatments are also emerging. In May 2023, the FDA approved ensifentrine, a new inhaler that reduces flare-ups by 15% and improves walking distance. Research is also looking at gene-based therapies to target mucus production directly - trials are already starting in 2024.
But none of these replace quitting smoking. The most cost-effective treatment? Smoking cessation. Every dollar spent on support programs saves $5.60 in healthcare costs within two years.
Living With Chronic Bronchitis - It’s Manageable
You can still live well. You can still travel, garden, play with grandkids, and walk the dog. But you have to be smart about it.Keep your home clean and dust-free. Use a humidifier if the air is dry. Avoid cold, dry weather - it triggers coughing. Dress warmly outside. Carry your rescue inhaler everywhere. And never ignore a sudden worsening of symptoms - that could be a flare-up that needs quick treatment.
It’s not about perfection. It’s about progress. One day at a time. One breath at a time.
Is chronic bronchitis the same as COPD?
Chronic bronchitis is one type of COPD - the other is emphysema. Both involve airflow blockage, but chronic bronchitis is defined by persistent cough and mucus production. Many people have both conditions at once. The term COPD covers them all.
Can I still smoke if I use an inhaler?
No. Inhalers help manage symptoms, but they don’t stop the damage smoking causes. Every cigarette you smoke keeps your lungs inflamed and speeds up the decline. Using an inhaler while smoking is like putting a bandage on a broken leg and still running marathons. Quitting is the only way to stop the progression.
How long does it take to see results after quitting smoking?
Within 72 hours, your bronchial tubes begin to relax and mucus starts to clear. After two weeks, circulation improves. By three months, lung function begins to recover - you’ll notice less coughing and more energy. After a year, your risk of heart disease drops by half. The longer you stay quit, the more your lungs heal.
Do I need oxygen therapy for life?
Not always. Some people only need oxygen during sleep or exercise. Others, especially those with advanced disease, need it 15+ hours a day. Your doctor will test your blood oxygen levels regularly. If your levels improve with quitting and rehab, you might be able to reduce or stop oxygen later. But if you’re still smoking, your need for oxygen will likely grow.
Is pulmonary rehab worth the effort?
Yes - more than any other treatment. People who complete rehab report better sleep, less anxiety, more independence, and fewer hospital visits. It’s not just about strength - it’s about learning how to live with your lungs. You’ll gain tools you can use for the rest of your life. And it’s covered by Medicare and most private insurers.
Can I ever stop taking my inhalers?
Maybe - but only under your doctor’s supervision. If you quit smoking, do rehab, and your symptoms improve, your doctor might reduce your dose. But stopping cold turkey can cause a flare-up. Never adjust your meds without talking to your care team first.
Next Steps - What to Do Today
If you’re reading this and you smoke:- Call a quitline today. In the UK, it’s NHS Smokefree at 0300 123 1044. In the U.S., it’s 1-800-QUIT-NOW.
- Ask your doctor about varenicline or nicotine replacement.
- Request a referral to pulmonary rehabilitation - it’s not optional, it’s essential.
- Get your flu shot and pneumococcal vaccine if you haven’t already.
- Write down one small goal: “I will not smoke today.” Then do it.
You’ve lived with this longer than you should have. But your lungs haven’t given up on you yet. And neither should you.
14 Comments
Madhav Malhotra
January 11 2026
Wow, this is so helpful! I have a cousin in Delhi who’s been coughing for 5 years and still smokes. I’ll share this with him - maybe the part about pulmonary rehab will make him listen. In India, we don’t have much access to these programs, but at least now I can tell him about the vaccines and quitting lines. Thank you for writing this with so much care ❤️
Jason Shriner
January 12 2026
so like... chronic bronchitis? more like chronic regret. you smoked for 40 years, now your lungs are a rusty vacuum cleaner. congrats. the real miracle? that you’re still alive.
ps: if you need a 12-week rehab program to learn how to breathe, maybe you should’ve thought about that before you turned your trachea into a ashtray.
Alfred Schmidt
January 12 2026
I’ve been reading this for 20 minutes and I’m already exhausted. You think I don’t know that smoking kills? I’ve lost three brothers to COPD. I’ve watched them choke on their own mucus while hooked to oxygen tanks. And now you’re telling me to ‘just quit’ like it’s a lifestyle change? It’s not. It’s a death sentence you signed with every cigarette.
And don’t get me started on those inhalers - half the people I know use them wrong. They puff like they’re trying to light a joint. I’ve seen people collapse in pharmacies because they didn’t know how to use a spacer. This isn’t healthcare. It’s a circus.
Roshan Joy
January 13 2026
This is such a balanced and practical guide! I especially appreciated the part about mucolytics - I didn’t know NAC was recommended by GOLD. I’ve been using it for 8 months now and my morning cough has dropped from 20 minutes to 5. Also, the oxygen therapy stats were eye-opening. My uncle was on 24/7 oxygen and now he’s down to 12 hours after quitting. 🙌
Michael Patterson
January 14 2026
The author clearly didn't understand the difference between correlation and causation. Just because 75% of chronic bronchitis patients are smokers doesn't mean smoking caused it - maybe it's the reverse? Maybe people with pre-existing lung issues are more likely to smoke? Also, the 60% decline stat - from what study? Was it a double-blind RCT? Or just a retrospective survey of people who were already motivated to quit? I’ve seen these numbers before - they’re always from pharma-funded trials. Also, why no mention of air pollution in urban areas? That’s a bigger factor than most admit.
Priscilla Kraft
January 15 2026
I’m a respiratory therapist and I just want to say thank you for mentioning pulmonary rehab. So many people think it’s just ‘exercise class’ - it’s not. It’s life-changing. We teach breathing retraining, pacing, nutrition, even how to manage anxiety. One of my patients, 72, went from needing oxygen to walk to the bathroom to walking 2 miles with no help. She cried when she got her first good night’s sleep in 10 years. 💙 If you’re reading this and you’re scared to start - just show up. The first session is always the hardest.
Christian Basel
January 15 2026
The entire premise is reductionist. Chronic bronchitis is a systemic inflammatory condition with epigenetic components, not a simple smoking-induced artifact. The reliance on bronchodilators and mucolytics is symptomatic palliation - not disease modification. The real therapeutic frontier lies in IL-1β and TNF-alpha inhibition, which are being explored in phase II trials. Also, the author ignores the role of gut-lung axis dysbiosis. Smoking alters microbiota, which modulates airway inflammation. No mention of probiotics? Pathetic.
Adewumi Gbotemi
January 16 2026
I live in Lagos and I see this every day. People cough all day, but they still smoke because they say it’s the only thing that calms them. This post is good, but in Nigeria, we don’t have clinics for rehab or even cheap inhalers. We need more than advice - we need access. Maybe someone can help get these resources to places like ours?
Jennifer Littler
January 17 2026
I’m a nurse who works in pulmonary. I’ve seen patients who quit smoking at 70 and lived another 15 years. I’ve also seen people who ‘only smoked a pack a day’ and died at 58. There’s no safe level. And yes, the inhalers? Most patients use them wrong. I’ve watched people inhale, then immediately exhale. No. You hold it. You wait. You breathe out slowly. It’s not intuitive. That’s why we have respiratory educators. They’re not optional. They’re essential.
Sean Feng
January 18 2026
Quit smoking. Done.
Vincent Clarizio
January 19 2026
You know what’s ironic? We spend billions on lung transplants for smokers who didn’t quit - but we won’t fund a single quitline for every high school student in America. This isn’t about health. It’s about control. The medical-industrial complex profits off chronic disease. They want you dependent on inhalers, oxygen, rehab, and endless doctor visits. But if you quit? They lose you. And that’s why they don’t scream it from the rooftops. They whisper it. In a blog. Like this. Don’t be fooled.
Sam Davies
January 19 2026
Ah yes, the classic ‘quit smoking’ sermon. How quaint. I’m sure the 18th-century physicians who recommended snuff for ‘lung vitality’ would be thrilled. But let’s be honest - this isn’t medicine, it’s moralism dressed in clinical jargon. The real tragedy? We’ve turned a physiological condition into a character flaw. You didn’t ‘fail’ your lungs. The system failed you. Where’s the housing policy? The air quality reform? The union-backed workplace protections? No. We blame the victim. Classic.
Alex Smith
January 21 2026
I’m a former smoker who quit at 52 after 30 years. This post nailed it. But here’s the thing nobody says: the first week after quitting? You feel like you’re dying. Your body’s screaming for nicotine. You cry over toast. You snap at your kids. You think, ‘I can’t do this.’ But you do. And then, one day, you realize you haven’t coughed in three days. And you walk up the stairs without stopping. And you smell flowers again. That’s the real cure. Not the inhaler. Not the rehab. You. Just you. And the choice you made.




Matthew Miller
January 11 2026
This post is basically a 2000-word ad for quitting smoking. Cool. But let’s be real - most people with chronic bronchitis aren’t sitting around reading medical blogs. They’re too busy wheezing through their third pack a day. And no, ‘just quit’ isn’t a treatment plan. It’s a cop-out.
Where’s the data on how many people actually *succeed* quitting after diagnosis? You cite 45% with support, but what’s the attrition rate at month 3? Month 6? Most of those numbers are cherry-picked from clinical trials with perfect compliance. Real life? People relapse. They get depressed. They smoke to cope. This post ignores the psychological hell of addiction. Just saying.