IBS: Understanding Symptoms, Triggers, and Management Strategies
When you have IBS, Irritable Bowel Syndrome is a common functional gastrointestinal disorder characterized by recurring abdominal pain and altered bowel habits without visible damage to the digestive tract. Also known as spastic colon, it doesn’t show up on scans or blood tests—but the pain and disruption to daily life are very real. Unlike Crohn’s or ulcerative colitis, IBS isn’t caused by inflammation or structural damage. It’s a brain-gut communication problem, where stress, food, or even gut bacteria can trigger signals that turn normal digestion into discomfort.
People with IBS often deal with bowel symptoms, including diarrhea, constipation, or switching between both, along with bloating and gas that can feel unbearable. These aren’t just "bad days"—they’re part of a pattern that can last for years. What makes IBS tricky is that triggers vary wildly. For one person, it’s coffee or dairy. For another, it’s stress, antibiotics, or even a high-FODMAP meal. The same foods that help one person can wreck another’s week. That’s why there’s no single cure, but there are proven ways to take control.
Gut health, the balance of bacteria and immune activity in the digestive tract, plays a central role in IBS. Studies show that people with IBS often have different gut microbes than those without it. Probiotics, fiber adjustments, and even low-FODMAP diets aren’t just trendy—they’re backed by data showing real symptom reduction. And while meds like antispasmodics or low-dose antidepressants are sometimes prescribed, many find relief through lifestyle tweaks: eating slower, managing stress with breathing exercises, or keeping a simple food-symptom log.
What you won’t find here is magic pills or miracle cures. What you will find are real stories and science-backed strategies from people who’ve lived with IBS long enough to know what works—and what doesn’t. From how to read medication labels when you’re on multiple gut meds, to understanding how antibiotics can mess with your gut for months, to figuring out if that new probiotic is worth the cost—this collection cuts through the noise. You’ll learn how to track your symptoms, recognize hidden triggers, and talk to your doctor without feeling dismissed. This isn’t about fixing IBS overnight. It’s about building a routine that lets you live with it, not be ruled by it.
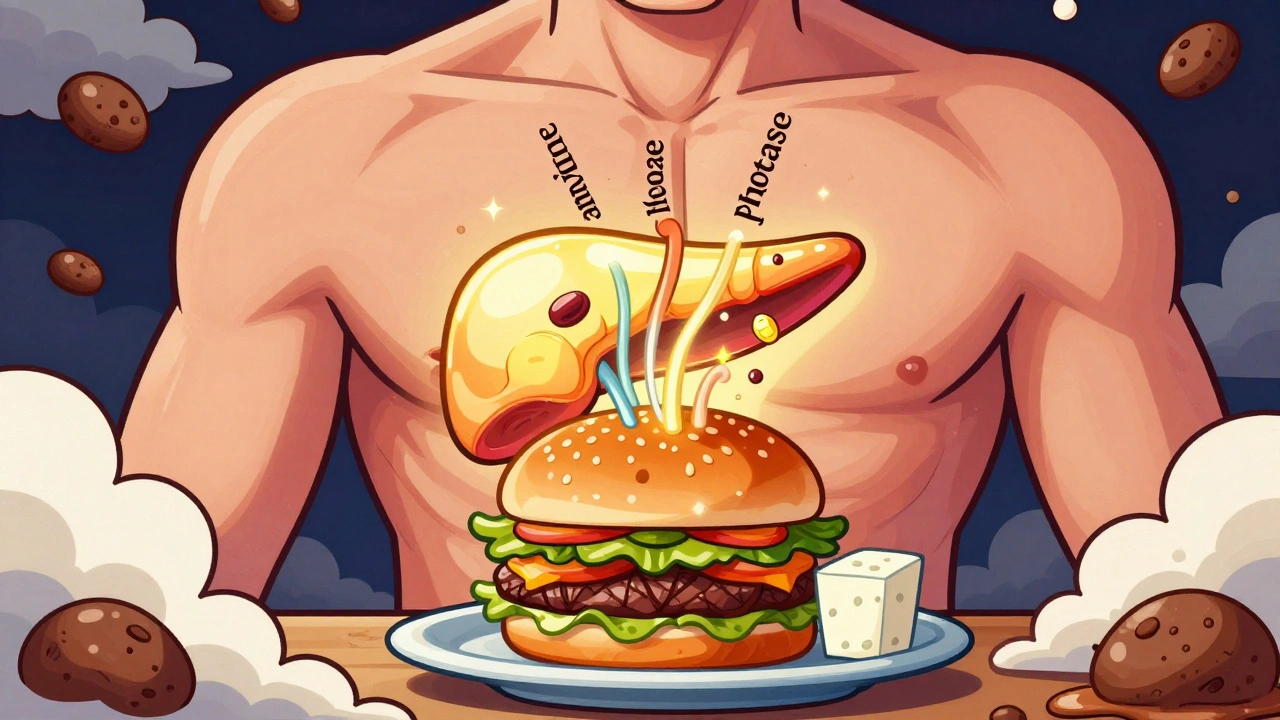
Digestive Enzymes: When Supplements May Help GI Symptoms
Digestive enzyme supplements may help with specific conditions like EPI or lactose intolerance, but often don't work for general bloating or IBS. Learn when they're effective, which types to choose, and when to skip them entirely.
View More