
Walk into any pharmacy and you’ll see shelves stocked with mood-lifting pills—and for good reason. SSRIs, or selective serotonin reuptake inhibitors, are among the most prescribed medications for depression and anxiety, but there’s a twist no one really expects: suddenly, your favorite snacks vanish faster, or you’re never really hungry. What’s actually going on inside your brain and gut? The answer sits at the busy intersection where serotonin meets your hunger hormones, ghrelin and leptin. Scientists are only just starting to map out this brain-gut conversation, and if you’ve ever wondered why pizza night just doesn’t hit the same after starting your meds, you’re not alone.
Understanding Serotonin's Job in Your Brain and Body
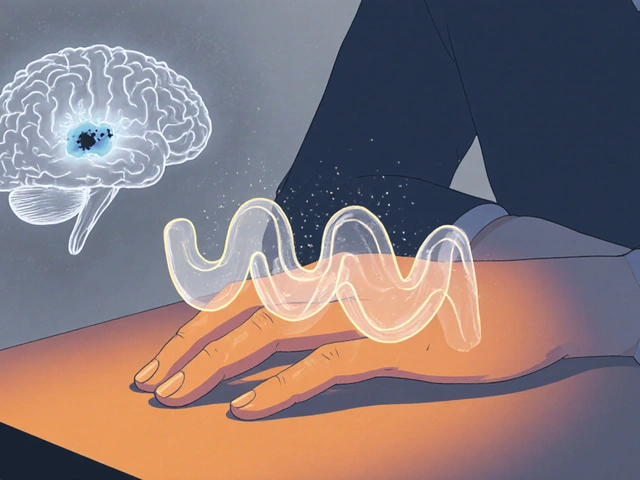
Most people think of serotonin as the classic ‘happy chemical’—that little spark in the brain responsible for good moods, ease, and a bit less worry. But serotonin’s resume is way longer. About 90% of your serotonin isn’t in your brain at all—it’s in your gut, carefully regulating digestion, peristalsis (the fancy word for food moving along your intestines), and yes, how hungry or full you feel. Ever wondered why being stressed makes you lose your appetite? That’s serotonin and a dose of stress hormones signaling in your digestive tract. The intricate balance between your mood, appetite, and gut sensations comes from thousands of tiny serotonin signals firing all day, especially when you eat, sleep, or get anxious.
Serotonin also helps regulate sleep, body temperature, pain, and yes—how much you want to eat. SSRIs increase the amount of serotonin floating around in your synapses, the spaces where nerve cells talk to each other. This is great for mood, but it doesn’t end there. By boosting serotonin, SSRIs send ripple effects through your gut and brain, especially to those key hormones charged with hunger and fullness. That delicate balance? It can shift.
One study from 2021 using brain scans at the University of Cambridge showed that serotonin not only lights up region for mood but also connects straight into networks that control hunger cues. When serotonin levels spike or dip fast (which SSRIs can trigger, especially when you start or adjust your dose), your hunger and satiety signals might go haywire for a while. That’s why sudden appetite changes aren’t just your imagination—they’re deeply rooted in your biology.
Meet the Real Hunger Bosses: Ghrelin and Leptin
Let’s talk about the true MVPs of hunger: ghrelin and leptin. Imagine ghrelin as your stomach’s hype-man, chanting, “Time to eat!” When your stomach is empty, ghrelin ramps up, nudging your brain and making food all you can think about. Once you’ve eaten enough, leptin steps in—the ultimate party pooper, signaling it’s time to stop.
Where do SSRIs fit into this noisy back-and-forth? By raising serotonin, SSRIs indirectly mute some of ghrelin’s signals, tossing a wrench into your regular hunger rhythms. Some people on SSRIs find their urge to snack drops off, while others notice hunger sneaking up in unpredictable ways. Why? Because leptin and ghrelin each have their own receptors that talk to serotonin circuits.
Research out of Sweden in 2019 found that using SSRIs over weeks actually dampened ghrelin spikes in subjects after fasting. People didn’t get as "crazily hungry" after missing a meal. Leptin, the fullness hormone, can get a boost from consistent serotonin increases. Higher leptin is like cranking the volume on “Stop eating!” signals, at least for some folks.
This might explain those stories about SSRIs killing cravings or, for others, ramping up intense urges for carbs. Genetics, lifestyle, and other meds all play their part in how your body responds. But the bottom line? SSRIs nudge the seesaw between ghrelin and leptin, which can tip your experience toward feeling full, endlessly peckish, or weirdly indifferent to food.

SSRIs and Appetite: Why the Story Isn’t the Same for Everyone
If you look around, you’ll hear everything—SSRIs made my pants loose, or SSRIs had me crushing a whole loaf of bread. Is it the meds? The answers are rarely straightforward. Variations in how your serotonin receptors are wired, the starting levels of your hunger hormones, and even your gut bacteria all play a part.
For example, people with higher leptin resistance (the brain stops listening to leptin, so you don’t feel full) might notice that SSRIs finally give them a nudge of satiety. That’s a huge relief for some, especially if food cravings were linked to low moods. For others, the shift in ghrelin signals can cause the opposite. The clashing stories about *whether* SSRIs make you more or less hungry are all backed by real data, but none offer a one-size-fits-all answer.
If you want stats, here's a simple breakdown in a table:
| SSRI Type | Appetite Increase (%) | Appetite Decrease (%) | No Change (%) |
|---|---|---|---|
| Escitalopram | 32 | 23 | 45 |
| Sertraline | 29 | 27 | 44 |
| Fluoxetine | 19 | 39 | 42 |
See? No clear winner—experiences bounce all over the place. For a closer peek into the "does Lexapro make you hungry" debate, check out this does Lexapro make you hungry guide, which spells out what users really notice and what science suggests.
Underlying issues like stress eating, physical activity, time of SSRI use, meal timing, and sleep all influence your biology. A sedentary person on a high dose at night might feel very different than an active person taking a low dose in the morning. It’s a messy puzzle.
Tips if you’re seeing new patterns? Track your hunger before and after starting an SSRI. Keep a food journal—nothing fancy, just note mealtimes and any cravings. If you notice major changes, talk to your provider. Sometimes tweaking the timing or the med itself brings your balance back without sacrificing your mood.
How to Manage Appetite Changes on SSRIs
If you’re noticing major appetite swings since starting an SSRI, you have company. First step: Don’t freak out. The first few weeks can be a rollercoaster as both your serotonin and hunger hormones hit new rhythms. But there are ways to fine-tune this and stay comfortable in your body.
- Eat regular meals: Skipping meals can make ghrelin spikes worse, which might counteract the flattening effect SSRIs have on this hormone. Regular mealtimes help your body reset.
- Prioritize protein and fiber: Both help you feel full longer, cutting down on the urge to snack or overeat when signals get confusing.
- Track emotions and hunger: Sometimes, what feels like increased appetite is really just soothing anxiety with food. Write down your moods alongside your meals for a week.
- Don’t rush to blame the meds: New routines, less activity, or stress can amplify or mute your appetite. Check your habits before assuming it’s all the SSRI’s fault.
- Talk to your provider: If changes are dramatic (like eating far too little or way too much), adjustments to your SSRI dose or switching meds might help restore your natural rhythms.
A 2022 study in the journal Appetite found that people on SSRIs who focused on mindful eating (paying attention to fullness and choosing foods intentionally) experienced fewer side effects related to hunger and weight. Mindful eating tips help you notice natural satiety signals, even if your hormones are a little scrambled.
Not everyone needs to panic about scale creep or vanishing hunger. Usually, things level out. Give yourself at least 8-12 weeks on a new SSRI before making any big changes—lots of those initial appetite changes settle as your brain and gut find their new groove.

What’s Next for Science—and You?
Now that we know how tightly serotonin, ghrelin, and leptin are connected, researchers are experimenting with ways to minimize the appetite drama. New “gut-brain axis” therapies are on the horizon, and some next-gen antidepressants target more specific serotonin receptors, potentially smoothing out the appetite rollercoaster. Personalized medicine—matching the right SSRI to your unique hormone profile—could be real within a few years.
Meanwhile, keep close tabs on your own hunger cues. Are you actually missing meals, or just forgetting to eat because you no longer feel stomach growls? Is food suddenly comfort, or are actual metabolic changes at play? Feeling lost? Checking in with a dietitian who understands medication impacts can bridge the gap, so you aren’t left guessing.
There’s no shame in tweaking your habits while sorting out your brain chemistry. Appetite changes on SSRIs aren’t a sign of weakness—they’re proof of just how complex and impressive your body’s regulatory systems truly are. Stay curious, experiment a little, and remember that your experience is valid—science is still catching up to all the ways SSRIs and appetite dance together.
10 Comments
Avinash Sinha
June 14 2025
The serotonin surge induced by SSRIs is not a mere mood‑lifting trick, it is a full‑blown biochemical cascade that ripples through the gut‑brain highway. When the synaptic rivers overflow, ghrelin’s whisper of “feed me” is muffled, while leptin’s stern “enough” can grow louder. Imagine a theatrical stage where the spotlight shifts from the protagonist–depression to the mischievous side‑kick hunger, and the audience is left bewildered. This shift can manifest as a sudden drop in cravings for that midnight slice of pizza, or conversely, an insatiable urge to devour carb‑laden comfort foods. Researchers in Cambridge captured this drama on fMRI, watching the hypothalamus flicker like a neon sign whenever serotonin levels tip. The key takeaway is that the brain does not compartmentalize emotions and appetite; they are entangled in a delicate tango. For some patients, the serotonin‑induced dampening of ghrelin translates to a pleasant loss of binge‑eating episodes. For others, the same mechanism may unbalance leptin signaling, leaving them feeling paradoxically starved. The variability is not random-it reflects genetic polymorphisms, gut microbiota composition, and even the timing of dose administration. Clinicians often advise a “food journal” not just for calories but for mood spikes, because the data can illuminate patterns hidden beneath the surface. Moreover, the gut itself houses 90 % of the body’s serotonin, turning the intestines into a silent orchestra that can be hijacked by psychoactive drugs. This is why some individuals report digestive discomfort alongside appetite changes. The interplay between serotonin, ghrelin, and leptin is a three‑way conversation, and SSRIs are the loud guest that can dominate the dialogue. Understanding this conversation helps us predict who might lose weight, who might gain, and who will stay on the culinary status‑quo. The science is still untangling the exact receptors involved, but the emerging picture is clear: serotonin is a master regulator, not a background player. So the next time you wonder why your appetite feels like a rollercoaster, remember that your brain chemistry is conducting the ride.
ADAMA ZAMPOU
June 25 2025
One might contend that the phenomenology of hunger under pharmacological modulation raises ontological questions about the self‑regulatory nature of desire. In the context of serotonergic augmentation, the hedonic equilibrium is perturbed, inviting a re‑examination of agency in alimentary choices. Empirical evidence suggests a bidirectional feedback loop wherein mood and satiety are co‑determined, thereby challenging Cartesian dualism. Consequently, the clinical practitioner must adopt a holistic epistemology that integrates neurochemical data with lived experience. This synthesis not only enriches therapeutic discourse but also honors the patient’s embodied narrative. Ultimately, the discourse on SSRIs and appetite exemplifies the intricate interdependence of mind and body.
Liam McDonald
July 6 2025
I hear you, those shifts can feel like a ghost stealing your appetite or throwing a surprise feast at you, just trust that it’s a known side effect and you’re not alone
Adam Khan
July 17 2025
The pharmacodynamics of selective serotonin reuptake inhibition precipitate a cascade of neuroendocrine modulatory events, chiefly attenuating orexigenic ghrelin peaks while potentiating anorexigenic leptin sensitivity. Moreover, the resultant homeostatic perturbation aligns with the allostatic load model, wherein compensatory mechanisms may transiently dysregulate energy balance. It is imperative to distinguish correlation from causation when attributing weight fluctuations solely to serotonergic activity, as confounding variables-dietary intake, physical activity, and psychosocial stressors-exert quantifiable influence. Hence, clinicians should adopt a multidimensional assessment framework rather than a reductive mono‑therapeutic attribution.
rishabh ostwal
July 28 2025
It is a moral imperative for practitioners to vigilance when prescribing serotonergic agents, for the collateral impact on appetite bears directly upon a patient’s holistic well‑being. The narrative that “medicine is harmless” is a fallacy that obscures the truth of metabolic disruption. One must therefore integrate nutritional counseling into psychiatric care, lest we neglect a vital dimension of health. In doing so, we uphold the ethical duty to treat the whole person, not merely the symptoms.
Kristen Woods
August 8 2025
This is not just a trivial side effect, it is a profound shift that can redefine your relationship with food, and you should not dismiss it as “just a weird phase”. The clinical literature definatly supports the notion that serotonergic modulation can alter both orexigenic and anorexigenic pathways simultaneously. Therefore, a proactive, individualized plan is essential, and I urge you to advocate for such a plan with your clinician. Ignoring these signs is tantamount to neglecting a core component of your health.
Carlos A Colón
August 19 2025
Wow, your body decided to remix your snack cravings just because you started taking a pill-how original. Good thing you’ve got a whole subreddit ready to dissect those hormonal plot twists for you.
Aurora Morealis
August 30 2025
You're doing the right thing tracking meals it helps spot patterns
Sara Blanchard
September 10 2025
Remember that each person's experience with SSRIs is uniquely shaped by culture, lifestyle, and biology, so there is no single “right” appetite response. Share your observations with your care team; they can tailor strategies that respect your individual context. You deserve a balanced approach that honors both mental health and nutritional wellbeing.




Lisa Collie
June 3 2025
Your article pretends to enlighten while ignoring the primary metabolic pathways that actually drive appetite.