Generic vs Brand Name Drugs: What You Really Need to Know
When you pick up a prescription, you might see two names on the bottle: one you recognize, and another that looks like a random string of letters. The first is the brand name drug, a medication originally developed and marketed by a pharmaceutical company under a patent. Also known as name-brand medication, it’s often expensive because the company recoups research costs. The second is the generic drug, a version made after the patent expires, containing the same active ingredient at the same strength and dosage. Also known as generic medication, it’s usually cheaper because manufacturers don’t repeat costly clinical trials. Both are required by the FDA to work the same way in your body—but that’s where the simplicity ends.
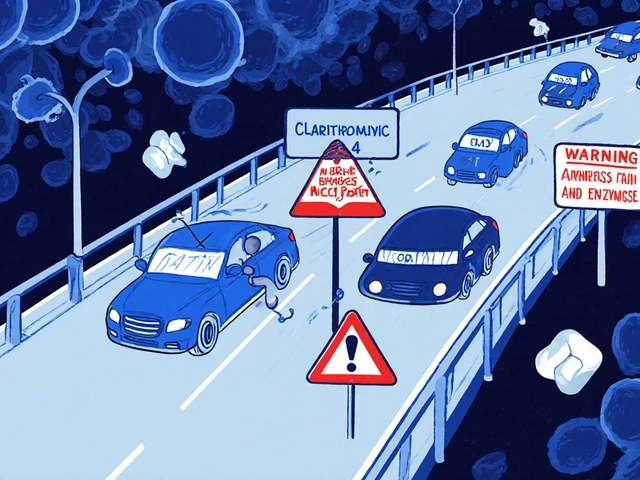
Here’s what most people don’t realize: generic vs brand name isn’t just about price. For most drugs, the difference is invisible. But for a small group of medications—like levothyroxine, warfarin, or phenytoin—tiny variations in fillers or absorption rates can matter. That’s why your doctor might ask you to stick with one brand if you have thyroid disease, heart issues, or epilepsy. These are called narrow therapeutic index drugs, and even a 5% change in how your body absorbs them can throw off your treatment. If you’ve switched generics and felt off, you’re not imagining it. That’s why keeping a medication journal, a personal log of how you feel after each refill. Also known as drug response tracker, it helps you spot patterns and talk to your doctor with real data. Some people notice side effects like headaches, fatigue, or mood shifts after switching. Others see no change at all. The key is tracking your own experience, not trusting assumptions.
And then there’s the dark side: contamination. Recent recalls have shown that some generic drugs—especially those made overseas—have contained cancer-causing chemicals like NDMA or benzene. These aren’t mistakes; they’re failures in quality control. That’s why knowing where your meds come from matters. Not every generic is equal. Some are made by the same companies that make the brand versions, just under a different label. Others are produced in factories with poor oversight. The FDA inspects, but not enough. If you’re on a long-term medication, ask your pharmacist: "Is this made in the U.S. or India?" It’s a simple question that can save your health.
You’ll find posts here that break down exactly which drugs need extra caution when switching, how to spot unsafe generics, and what to do if you feel worse after a refill. We cover real cases—from thyroid patients who had to go back to Synthroid, to people who switched from brand-name Plavix and ended up in the ER. You’ll also see comparisons of generic alternatives like Zenegra vs. Viagra, or Soolantra vs. metronidazole, so you know what’s actually worth saving money on—and what’s not. This isn’t about fear. It’s about control. You have the right to understand what’s in your body. These articles give you the facts to make smart choices, not just cheap ones.

Cardiovascular Generics: What Safety Studies and Real-World Data Really Show
Cardiovascular generics save billions but aren't always equal. Real-world data shows mixed safety results-some work fine, others trigger side effects. Here's what the studies and patient experiences reveal.
View More