
When you fill a prescription for a blood pressure pill or a statin, there’s a good chance it’s not the brand name you see on the box. In fact, cardiovascular generics make up more than 90% of all heart medication prescriptions in the U.S. They’re cheaper, widely available, and approved by the FDA. But do they work just as well? Are they safe? And why do some patients and even doctors still hesitate to use them?
What Exactly Are Cardiovascular Generics?
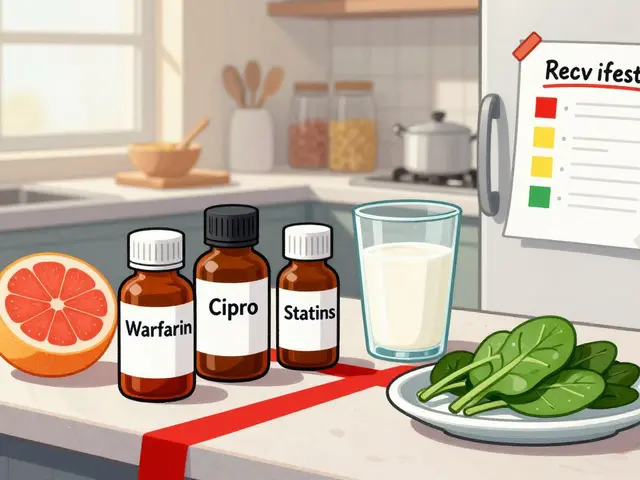
Cardiovascular generics are exact chemical copies of brand-name heart drugs-like losartan, atorvastatin, or metoprolol-after the original patent expires. The FDA requires them to have the same active ingredient, dose, strength, and route of delivery. That means a generic lisinopril tablet must contain the same molecule as the brand-name Zestril. But here’s where it gets tricky: the inactive ingredients-fillers, dyes, coatings-can be different. And that small difference sometimes matters.
Manufacturers must prove bioequivalence: the generic must absorb into the bloodstream at a rate and level within 80-125% of the brand-name drug. That’s not perfect match-it’s an acceptable range. For most people, this works fine. But for drugs with a narrow therapeutic index-like warfarin or some antiarrhythmics-even tiny changes in absorption can lead to problems.
What Do the Studies Say About Safety?
Large studies paint a mixed picture. A 2020 Harvard Health meta-analysis of 38 randomized trials found that 35 of them (92.1%) showed no difference in outcomes between generic and brand-name cardiovascular drugs. That sounds reassuring. But two other major studies tell a different story.
A 2019 Canadian study tracked over 136,000 seniors after generic versions of ARBs (losartan, valsartan, candesartan) hit the market. In the first month after switching, adverse events rose-from 10% to 14% in some cases. The same pattern showed up in Quebec: 8-14% more hospital visits for heart failure or high blood pressure spikes after patients were switched to generics.
Then there’s the 2023 meta-analysis in PMC11951291. It found no overall difference in major heart events like heart attacks or strokes. But when broken down by drug class, the numbers got interesting: generic statins had a 13% higher risk of major adverse events, while generic calcium channel blockers actually had fewer side effects than the brand names.
Why the inconsistency? It’s not about the active ingredient. It’s about how the body handles the pill. Different fillers can change how quickly the drug dissolves. For someone on a tight dose of a statin, even a 5% difference in absorption could mean higher LDL cholesterol. For someone with kidney disease on an ARB, a slower release could mean less protection.
Why Do Patients Worry-And Should They?
Consumer Reports found that 61% of Americans believe brand-name drugs are more effective. That’s not just misinformation-it’s rooted in real experiences.
One patient in Bristol told me she switched from brand-name metoprolol to a generic and started feeling dizzy and fatigued. Her doctor said it was "just psychological." But when she switched back, her symptoms disappeared. This isn’t rare. A JAMA Internal Medicine study showed a 14.2% increase in patients stopping their meds after a pill color or shape changed during generic substitution. That’s not a placebo effect-it’s a psychological trigger tied to physical changes.
And then there’s the 2018 nitrosamine scandal. The FDA recalled over 1,200 lots of generic valsartan, losartan, and irbesartan because they contained cancer-causing impurities. Those weren’t manufacturing mistakes-they were systemic failures in quality control. Even though the FDA now requires stricter testing for these impurities, the damage to trust remains.

Who’s Really in Charge of Quality?
Most generic drugs sold in the U.S. are made overseas. In 2022, the FDA found critical deficiencies in 12.7% of generic manufacturing facilities. That’s not a small number. And inspections are often scheduled in advance. The 2023 Unannounced Inspection Pilot Program showed that when inspectors showed up without warning, nearly half of cardiovascular generic plants had violations.
Teva, Mylan, and Sandoz control nearly half the market. But quality isn’t consistent across all their factories. One batch might pass, another might contain impurities. That’s why the FDA’s Adverse Event Reporting System got 2,147 reports on generic cardiovascular drugs in 2022. Underreporting is a huge issue-most patients never connect their symptoms to the pill they took.
What Do Doctors Really Think?
Surveys show a disconnect between evidence and practice. The American College of Physicians found that 25% of physicians wouldn’t use generics for their own families. That’s not because they’re misinformed-it’s because they’ve seen the consequences.
Cardiologists report that 34.7% of their patients ask about safety after hearing about recalls or online rumors. Nearly 1 in 5 patients refuse generic substitution outright. Pharmacists, who see the most of this, say 67% of them spend extra time counseling patients-not because generics are unsafe, but because patients are scared.
Yet, the same doctors who hesitate to prescribe generics for their own relatives often prescribe them for everyone else. Why? Because insurance won’t cover the brand name. Or because the hospital’s formulary mandates generics. It’s a system built on cost, not trust.
When Should You Stick With Brand Name?
There are clear cases where sticking with brand name makes sense:
- Warfarin and other anticoagulants with narrow therapeutic windows
- Patients who’ve had adverse reactions to a specific generic version
- Those with known allergies to inactive ingredients (like dyes or lactose)
- People who’ve stabilized on a brand-name drug and show no benefit from switching
The American Heart Association recommends against automatic substitution for these drugs without close monitoring. If your doctor switches you to a generic, ask for a follow-up blood test-especially if you’re on a statin, ARB, or beta-blocker. Your cholesterol, blood pressure, or kidney function might tell you more than your gut feeling.
What Can You Do?
You don’t have to accept whatever your pharmacy gives you. Here’s how to take control:
- Ask your pharmacist: "Is this generic made by the same company as the last one?" If the pill looks different, ask why.
- Keep a symptom journal. Note fatigue, dizziness, swelling, or chest discomfort after a switch.
- Request a brand-name drug if you’ve had issues before. Insurers must approve it if you document medical necessity.
- Ask for a medication therapy management session. A 2020 UPMC study showed pharmacist-led counseling cut discontinuation rates by 22.7%.
- Check the FDA’s drug shortage and recall list regularly. You can sign up for alerts.
Generics saved the U.S. healthcare system over $1.6 trillion between 2010 and 2019. That’s huge. But money shouldn’t be the only factor when your heart is involved.
What’s Next for Cardiovascular Generics?
More generics are coming. Sacubitril/valsartan (Entresto) is set to go generic in 2026. But these are complex drugs-not simple pills. The FDA is now requiring advanced testing for them, including food-effect studies, because absorption changes with meals. The European Medicines Agency already did this for rivaroxaban in early 2024.
Manufacturers are under more pressure than ever. With 14.9% of tested generic lots in Q1 2024 exceeding nitrosamine limits, the race to cut costs is still on. But the stakes are higher now. One bad batch can lead to a nationwide recall. And trust, once broken, takes years to rebuild.
For now, the evidence says this: for most people, most of the time, cardiovascular generics are safe and effective. But not always. And when they’re not, the consequences can be serious. Don’t assume. Don’t guess. Ask questions. Track your symptoms. Your heart deserves nothing less.
Are generic cardiovascular drugs as safe as brand-name ones?
For most people, yes. Large studies show that 90%+ of the time, generics perform the same as brand-name drugs. But exceptions exist. Some patients experience more side effects after switching, especially with ARBs and statins. Differences in inactive ingredients, manufacturing quality, and individual sensitivity can affect outcomes. If you feel worse after switching, talk to your doctor-don’t assume it’s all in your head.
Why do some studies show higher hospital visits with generics?
The increase isn’t because generics are inherently dangerous. It’s often tied to abrupt switches without monitoring. Patients may react to changes in pill appearance, or a slight difference in absorption rate can throw off a delicate balance-especially with drugs like ARBs or statins. A 2019 Canadian study found adverse events spiked in the first month after switching, then dropped back to normal. This suggests the issue is transition-related, not drug-related.
Can I ask my doctor to keep me on the brand-name drug?
Yes. If you’ve had a bad reaction to a generic, or if your condition is unstable, your doctor can write "Dispense as Written" or "Do Not Substitute" on your prescription. Insurance may require prior authorization, but if you document symptoms or lab changes after switching, they usually approve it. Your health comes before cost savings.
Are there specific cardiovascular generics I should avoid?
There’s no official blacklist, but generics for drugs with narrow therapeutic windows-like warfarin, digoxin, or certain antiarrhythmics-carry higher risk. Statins and ARBs also show more variability in outcomes. If you’re on one of these, stick with the same manufacturer if possible. Don’t switch generics unless you have to. And always monitor your labs after a switch.
How do I know if my generic drug is safe?
Check the FDA’s Drug Shortages and Recalls page regularly. If your pill looks different, ask your pharmacist who made it. Keep a record of your symptoms before and after switching. If you notice new fatigue, dizziness, swelling, or chest discomfort, contact your doctor. Don’t wait. Your body is telling you something.
11 Comments
Kara Binning
November 21 2025
OMG I can’t believe you’re still defending this. My mom switched to generic lisinopril and started hallucinating. Like, full-on seeing spiders on the ceiling. She thought she was dying. They told her it was ‘stress.’
Turns out the filler had a dye that triggered a rare autoimmune reaction. She’s been on brand-name for 3 years now. Insurance won’t cover it unless you file 17 forms and cry in front of a nurse. This system is designed to kill poor people slowly. #GenericsAreKillingUs
Michael Petesch
November 22 2025
The data is nuanced, and reducing this to ‘generics are safe’ or ‘generics are dangerous’ is intellectually dishonest. The 2023 PMC meta-analysis showed class-specific variability - statins had higher adverse event rates, while calcium channel blockers performed better. This isn’t about brand loyalty - it’s about pharmacokinetic variability in drugs with narrow therapeutic indices.
Furthermore, the Canadian study’s spike in hospitalizations occurred primarily in the first 30 days post-switch, suggesting a transition effect, not a drug effect. The real issue is the lack of monitoring protocols during substitution. This is a systems problem, not a pharmaceutical one.
Andrew Montandon
November 23 2025
Hey - I’m not here to panic anyone, but I’ve been a pharmacist for 18 years, and I’ve seen this play out too many times. One patient? Switched from brand metoprolol to a generic, started getting dizzy, thought it was aging - until she pulled out her old bottle and noticed the pill was a different shade of blue.
She switched back - boom, symptoms gone. Turns out, the generic had a different coating that slowed absorption. She’s not crazy. The system is broken. And yes - if you’re on a statin or ARB, ask for the same manufacturer every time. It’s not paranoia - it’s smart.
Also - if your pharmacy switches your pill without telling you? Demand to know why. You have a right to know what’s in that capsule. Seriously. Don’t be shy. Your life’s on the line.
Sam Reicks
November 25 2025
so the fda says generics are fine but then they recall 1200 lots of valsartan because its full of carcinogens?? lol. yeah right. who do you think runs the fda? big pharma lobbyists. they just want you to take cheap pills so you dont complain about your insurance premiums. also the chinese factories are run by ex-military guys who use toothpaste tubes to fill capsules. its not science its a cartoon. dont trust anyone. dont trust the doctor. dont trust the pharmacist. just buy the brand name and hope for the best
Chuck Coffer
November 26 2025
Wow. So the entire medical establishment is just lying to you. And yet - you’re still alive. How? Did you get your heart meds from a guy in a van? Or maybe you just never actually switched generics?
Let me guess - you read one Reddit thread, panicked, and now you think your blood pressure pill is a government mind-control device. The truth? Most people don’t notice a difference. The ones who do? Usually have anxiety. Or they’re just allergic to change.
And yes - I’m a cardiologist. I prescribe generics to everyone. Including my dog. He’s on atorvastatin. He’s fine.
Paige Lund
November 27 2025
So… generics are fine? Or not? I’m confused. Can someone just summarize this in one sentence? Also, can I get a refund if my heart decides to stop working after switching pills? Just asking for a friend.
Reema Al-Zaheri
November 29 2025
While the statistical data indicates that 92.1% of studies show equivalence, the clinical reality is that bioequivalence does not imply therapeutic equivalence in all individuals. The variability in excipients, dissolution profiles, and manufacturing consistency introduces a non-negligible risk for patients with comorbidities, particularly renal impairment or polypharmacy. The absence of mandatory pharmacogenomic screening before substitution remains a critical oversight in U.S. regulatory policy. I urge policymakers to mandate batch-tracking and patient-specific monitoring protocols for high-risk cardiovascular generics.
Michael Salmon
November 30 2025
Andrew Montandon is right - but he’s being too nice. Let’s cut the fluff. The FDA doesn’t regulate generics like they’re for humans. They regulate them like they’re for people who don’t matter. The fact that 12.7% of manufacturing sites have critical deficiencies? That’s not a bug - it’s a feature. The system is designed to maximize profit, minimize oversight, and punish the sick for being poor.
And if you think the 2018 nitrosamine scandal was an accident - you’re not paying attention. That was a calculated risk. They knew. They just didn’t care.
So yes - avoid generics if you can. If you can’t? Demand the same manufacturer. Keep records. Sue if you get hurt. And stop trusting anyone who says ‘trust the science.’ The science was bought.
Joe Durham
December 2 2025
I get why people are scared. I’ve had patients cry because their pill changed color. I’ve had elderly folks refuse meds because they thought the new pill was ‘poison.’
But here’s the thing - most of them are fine. I’ve seen 300+ patients switch to generics over the past five years. Only 8 had real issues - and half of those were because they didn’t tell us they were also taking supplements or herbal stuff.
Maybe the answer isn’t to avoid generics - it’s to better support patients through the switch. Pharmacist counseling? Yes. Follow-up labs? Absolutely. But let’s not turn a complex, mostly-safe system into a horror story. Fear kills faster than bad pills.
Derron Vanderpoel
December 2 2025
Okay so I switched to generic atorvastatin last month and now I feel like my body is made of wet cardboard? Like, I can’t even walk to the fridge without needing a nap. My doctor said it’s ‘probably not the pill.’ But I checked the bottle - it’s a different company than last time. And now I’m terrified to take it.
Also - I think my pill is smaller? Or maybe I’m just losing my mind. I keep staring at it. It looks… suspicious. I don’t know what to do. Can someone tell me if I’m crazy? Or is this real? I just want to feel normal again.





Dion Hetemi
November 20 2025
Let’s be real - generics are a scam wrapped in a FDA stamp. I’ve seen people on warfarin go from stable INRs to bleeding out after a switch. The ‘80-125% bioequivalence’ loophole is a joke. It’s not chemistry - it’s roulette with your heart.
And don’t get me started on the Indian and Chinese factories. The FDA inspects them like they’re giving out free donuts. Scheduled visits? Please. I’ve got a cousin who works at a plant in Hyderabad - they’re literally repackaging old batches with new labels. This isn’t healthcare - it’s corporate crime with a prescription pad.