More than 9 in 10 prescriptions in the U.S. are filled with generic drugs. They’re cheaper, widely available, and often just as effective as brand-name versions. But behind that convenience lies a growing crisis: contamination in generic medications is no longer rare-it’s becoming routine. From cancer-causing chemicals in blood pressure pills to toxic fumes in cough syrup, recent cases show that safety gaps in the global supply chain are putting patients at risk.
What’s Really in Your Generic Pills?
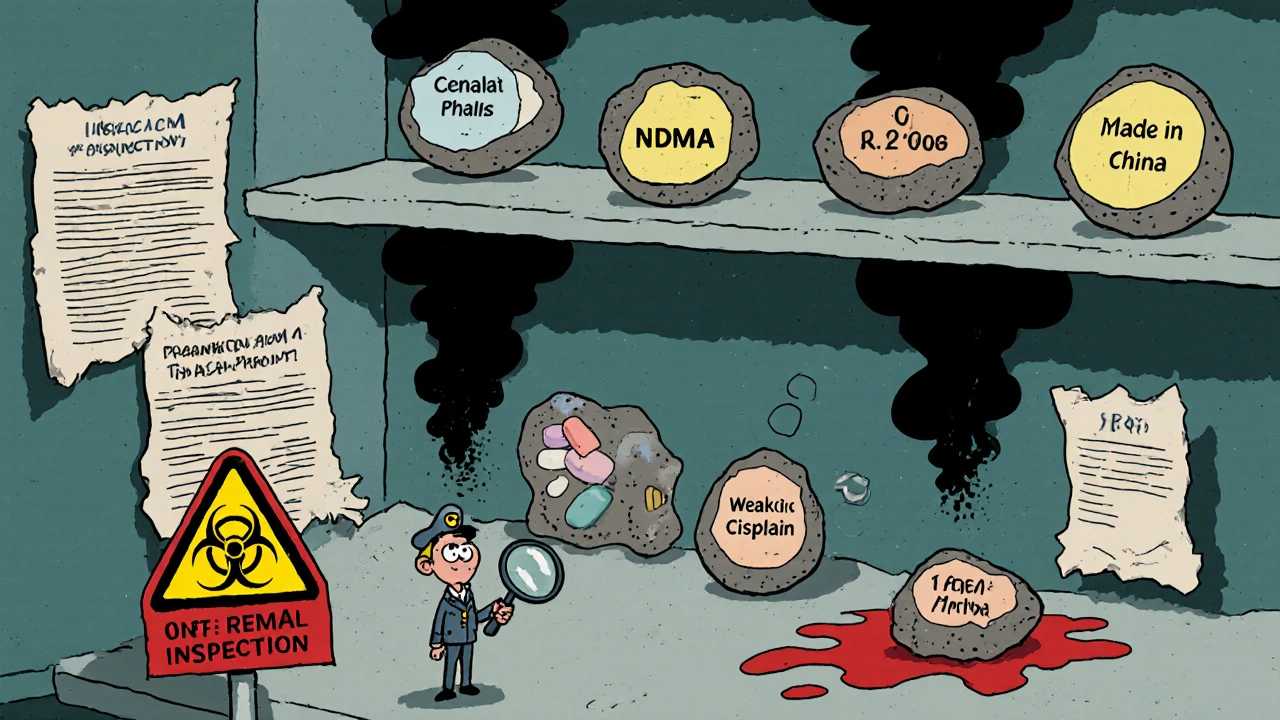
Generic drugs are supposed to be identical to their brand-name counterparts in active ingredients, dosage, and effectiveness. But they’re not made the same way. Most are produced in factories overseas-mainly in India and China-where cost-cutting often overrides quality control. In 2024, India supplied 40% of all finished generic drugs sold in the U.S., while China produced 80% of the active pharmaceutical ingredients (APIs) used in them. The problem isn’t just about missing ingredients. It’s about dangerous ones that shouldn’t be there at all. In 2018, the FDA found NDMA-a known carcinogen-in batches of the blood pressure medication valsartan. Levels in some pills were 200 times higher than the safe daily limit of 96 nanograms. That single contamination triggered over 1,300 lawsuits by September 2025, with patients developing cancer at more than three times the expected rate. The source? A simple, unapproved change in the manufacturing process at Zhejiang Huahai Pharmaceutical: sodium nitrite was added to reduce costs, but it reacted with other chemicals to form NDMA. Then came benzene in Mucinex. Independent lab tests found concentrations up to 4.7 parts per million in some generic versions-more than double the FDA’s legal limit of 2 ppm. Benzene is a known cause of leukemia. Two women in Chicago filed suit in June 2025 after developing bone marrow damage following 18 months of daily use. The manufacturer, Walgreens, had sourced the product from a facility with a history of quality violations. Oncology drugs are especially vulnerable. A 2025 STAT News investigation tested 17 chemotherapy drugs from Indian manufacturers. Twelve of them contained less than 80% of the labeled active ingredient. The FDA’s acceptable range is 85% to 115%. One batch of cisplatin from Intas Pharmaceuticals was so weak that 7 out of 11 patients in a Memorial Sloan Kettering study failed to achieve remission. The FDA later found that the factory had shredded quality control records and poured acid on them to destroy evidence.Why Do These Contaminations Keep Happening?
The root cause isn’t one bad actor-it’s a broken system. The FDA approves generic drugs based on bioequivalence studies, not full clinical trials. That’s efficient, but it doesn’t catch contamination. Once a drug is approved, inspections are rare. In 2025, the FDA inspected just 13% of Indian manufacturing plants, even though those facilities produce nearly half of all U.S. generics. There are over 28,000 foreign drug factories on the FDA’s radar-and only $78 million in the 2025 budget to inspect them. Manufacturers face enormous pressure to cut costs. The generic drug market is fiercely competitive. A single batch of a popular medication can be produced by dozens of companies. If one plant can make it cheaper-even if it cuts corners-they win the contract. And when a hospital or pharmacy switches suppliers for savings, they may never know the new batch is contaminated. Transparency is another issue. The FDA has long redacted the names of drugs linked to violations in inspection reports. That meant doctors and pharmacists couldn’t tell which specific generics were unsafe. It wasn’t until September 2025 that the agency announced a new “Name Transparency Initiative” to stop hiding drug names. But implementation is still uncertain.
Who’s Most at Risk?
Patients taking long-term medications are the most vulnerable. Someone on valsartan for high blood pressure might take it for 10, 15, or 20 years. Even small doses of NDMA over time can cause DNA damage. Patients on chemotherapy have no room for error. If a dose of cisplatin is 20% weak, the cancer may not respond. That’s not a minor mistake-it’s life or death. Opioid patches are another silent danger. Between 2002 and September 2025, over 52 million fentanyl patches were recalled due to seal failures. In one 2023 recall by Sandoz, 0.8% of Duragesic patches leaked more than 15% of their intended dose. That’s enough to cause an overdose in someone who’s opioid-tolerant-and potentially kill someone who isn’t. Patients aren’t always told when their medication changes. A Reddit user named PharmTech2020 reported seeing three different batches of generic levothyroxine fail potency tests in six months. Patients’ TSH levels spiked until pharmacists switched them back to the brand. No one warned them.What’s Being Done to Fix This?
The FDA has tried. The Pharmaceutical Quality for the 21st Century initiative, updated in 2023, pushes manufacturers to use real-time monitoring tools called Process Analytical Technology (PAT). These systems can detect contamination as it happens. But only 37% of foreign plants use them. In the U.S., 12% of facilities use continuous manufacturing-a method that reduces contamination risk by 78%-but only 3% of Indian plants do. The Drug Supply Chain Security Act (DSCSA) requires full electronic tracking of every drug package by 2027. Right now, only 62% of pharmacies can verify if a drug’s history is legitimate. That means a contaminated batch can move from a factory in Ahmedabad to a pharmacy in Des Moines without anyone knowing. New rules under GDUFA III, introduced in June 2025, now require real-time stability testing for high-risk drugs like chemotherapy and blood pressure medications. That’s a step forward. But penalties for violations are still weak. Zhejiang Huahai Pharmaceutical, the source of the valsartan NDMA contamination, was fined $1.2 million in 2025. That’s less than 0.1% of their annual revenue.
What Can You Do?
You can’t control the factory, but you can control what you take.- Check recall lists weekly. Pharmacists spend 22% more time now verifying drug sources. You should too. Visit the FDA’s website and sign up for recall alerts.
- Ask your pharmacist if your generic is from a U.S.-based manufacturer. While most APIs come from abroad, some finished drugs are packaged in the U.S. under stricter oversight.
- Don’t assume all generics are the same. Two brands of metformin might have different fillers or manufacturing processes. If your blood sugar suddenly behaves differently after a refill, speak up.
- Report side effects. If you suspect contamination-unusual symptoms, sudden changes in effectiveness, or visible particles in the pill-report it to the FDA’s MedWatch program.
- Consider brand-name drugs for critical medications. If you’re on chemotherapy, thyroid medication, or a blood thinner, the cost difference might be worth the safety margin. Many insurance plans still cover brand-name drugs if your doctor documents medical necessity.
The Bigger Picture
The generic drug system was built to save money-and it has. Over the past decade, generics saved the U.S. healthcare system $1.7 trillion. But that savings came at a cost: trust. Patients expect their pills to be safe. They don’t expect to be part of an experiment. The FDA is catching up. AI-powered analytics and blockchain tracking are coming. But until manufacturers face real consequences-fines that hurt, inspections that surprise, and transparency that protects-contamination will keep happening. For now, awareness is your best defense. Know what you’re taking. Question changes. Demand answers. Your health depends on it.Are generic drugs less safe than brand-name drugs?
Generic drugs are required by law to contain the same active ingredient as brand-name drugs and work the same way. But they can be made in different factories, with different processes, and different quality controls. Contamination issues have been found in generics more often than in brand-name drugs-not because the active ingredient is weaker, but because manufacturing oversight is looser, especially overseas.
Which generic drugs have been most affected by contamination?
Blood pressure medications like valsartan, losartan, and irbesartan (ARBs) have seen the highest number of contamination recalls due to NDMA. Chemotherapy drugs like cisplatin and carboplatin from Indian manufacturers have failed potency tests. Respiratory drugs like Mucinex have been found with benzene. Fentanyl patches have been recalled for seal failures. These are the most common and dangerous cases reported since 2018.
How can I tell if my generic drug has been recalled?
Check the FDA’s Drug Recalls page regularly. You can also sign up for email alerts. If your pharmacy switches your prescription to a different generic brand, ask them for the manufacturer’s name and lot number. You can then search for recalls using that information. Don’t rely on your pharmacist to catch every recall-do your own check.
Is it worth paying more for brand-name drugs?
For medications where precision matters-like thyroid hormone, seizure drugs, blood thinners, or chemotherapy-yes. A small variation in dose can have serious consequences. If your insurance covers the brand or you can afford the extra cost, it may be worth the peace of mind. Talk to your doctor about medical necessity.
Why does the FDA allow drugs from countries with poor oversight?
The U.S. doesn’t produce enough active ingredients or finished drugs to meet demand. China and India supply the bulk at lower prices. The FDA has limited resources to inspect thousands of foreign facilities. Until the U.S. invests in domestic manufacturing or enforces stricter penalties, the system will keep relying on overseas production-even when risks are known.
What’s being done to improve generic drug safety?
The FDA is moving toward real-time testing for high-risk drugs, requiring electronic tracking of every drug package by 2027, and stopping the practice of hiding drug names in inspection reports. Some manufacturers are adopting continuous manufacturing and AI monitoring. But progress is slow. Without stronger penalties and more inspections, these changes may not be enough.
19 Comments
Eleanora Keene
November 13 2025
I’ve been a pharmacist for 18 years, and I can tell you-this isn’t new. We’ve been warning people for years. But no one listens until someone they know gets sick. Please, just ask for the manufacturer name. It’s not that hard.
Joe Goodrow
November 15 2025
Let’s be real-this is what happens when you outsource everything to countries that don’t care about your kids. We used to make medicine here. Now we’re buying poison from factories that don’t even wash their hands before packaging. Time to bring it back home. America First, not America Poisoned.
Don Ablett
November 16 2025
It is noteworthy that the FDA's inspection regime remains grossly inadequate relative to the volume of imported pharmaceuticals. The statistical probability of undetected contamination increases exponentially with the number of unmonitored facilities. One must question the efficacy of regulatory capture in this domain.
Peter Aultman
November 17 2025
My grandma’s levothyroxine went nuts last year. TSH spiked, she was exhausted, dizzy. We switched back to Synthroid and boom-back to normal. No one told us the generic was different. That’s wild. Just check your bottle next time.
Nathan Hsu
November 19 2025
As an Indian citizen, I feel deeply hurt by these generalizations. Yes, some factories cut corners-but so do many in the U.S. We produce 40% of the world’s generics with pride and precision. The real issue is underfunding and greed-not nationality. Please don’t blame us for America’s broken system.
Ashley Durance
November 20 2025
People who buy generics are basically gambling with their lives. If you can’t afford the brand, maybe you shouldn’t be on expensive meds at all. It’s not the manufacturer’s fault-you’re the one choosing the risk. Sad, but true.
Scott Saleska
November 22 2025
Wait, so you’re telling me I’ve been taking a 20% weaker version of my chemo drug for 8 months? And no one told me? I’m going to the hospital right now. This is criminal. Someone needs to go to jail for this.
Kevin Wagner
November 23 2025
Y’all are acting like this is a surprise. We’ve known since 2012 that Indian and Chinese factories were cutting corners. The FDA’s been asleep at the wheel. But hey-when your insurance pays $3 for a pill instead of $300, you’re basically signing up for a Russian roulette round with your organs. Wake up, people.
gent wood
November 24 2025
This is a systemic failure of oversight, not an isolated incident. The commercial imperative to reduce cost has superseded the ethical imperative to ensure safety. We must advocate for structural reform-not merely individual vigilance. The burden should not rest on the patient.
Dilip Patel
November 26 2025
USA is the real problem here-always blaming others. We make medicine for the world and you still cry like babies. You don’t pay enough for quality, now you blame us? You want safe pills? Pay more. Simple. No more whining.
Jane Johnson
November 26 2025
Brand-name drugs are not inherently safer. The active ingredient is identical. The problem is batch variation, not origin. This narrative is misleading and fearmongering.
Sean Hwang
November 28 2025
My cousin works at a pharmacy. They get a new batch every week and they don’t even check the lot numbers unless someone complains. This is a mess. Just ask your pharmacist to show you the manufacturer. It’s not that hard.
Barry Sanders
November 28 2025
Of course the FDA is hiding names. They don’t want panic. But now people are dying. That’s not ‘regulatory caution’-that’s cover-up. And the media’s too scared to call it out. Pathetic.
Chris Ashley
November 30 2025
So what? I’ve been taking generic metformin for 5 years. No issues. You’re all overreacting. Stop being paranoid.
kshitij pandey
December 1 2025
India is proud of its pharmaceutical legacy. We are the pharmacy of the world. But yes, some bad apples exist. Let’s not throw the whole basket away. Support good manufacturers, report bad ones. We’re with you.
Brittany C
December 1 2025
Process Analytical Technology (PAT) and continuous manufacturing are not widely adopted due to capital expenditure constraints and regulatory uncertainty. The cost-benefit analysis for foreign manufacturers remains unfavorable without enforceable incentives.
Anjan Patel
December 2 2025
They don’t care. They know people are desperate. They know you’ll take it because you can’t afford the brand. They’re not evil-they’re just rich. And you? You’re the sucker who keeps buying.
Scarlett Walker
December 3 2025
I switched my dad to brand-name blood thinner after his stroke. He’s been fine for 14 months now. I wish I’d done it sooner. Don’t wait for a crisis. Ask your doctor. It’s worth it.






Ryan Anderson
November 12 2025
Just took my valsartan this morning. Saw the recall notice last week and switched to the brand. Worth every extra dollar. My BP hasn't been this stable in years. 🙌