Drug Interaction Checker
Check Your Medications
Results
Every year, thousands of people end up in the hospital not because their medication stopped working, but because it started working too well. This isn’t a rare mistake-it’s a predictable outcome of drug interactions. When two or more medications mix in your body, they don’t just sit there quietly. They fight, boost, or block each other, turning a mild side effect into a life-threatening one.
Why Your Medicine Might Be Making You Sicker
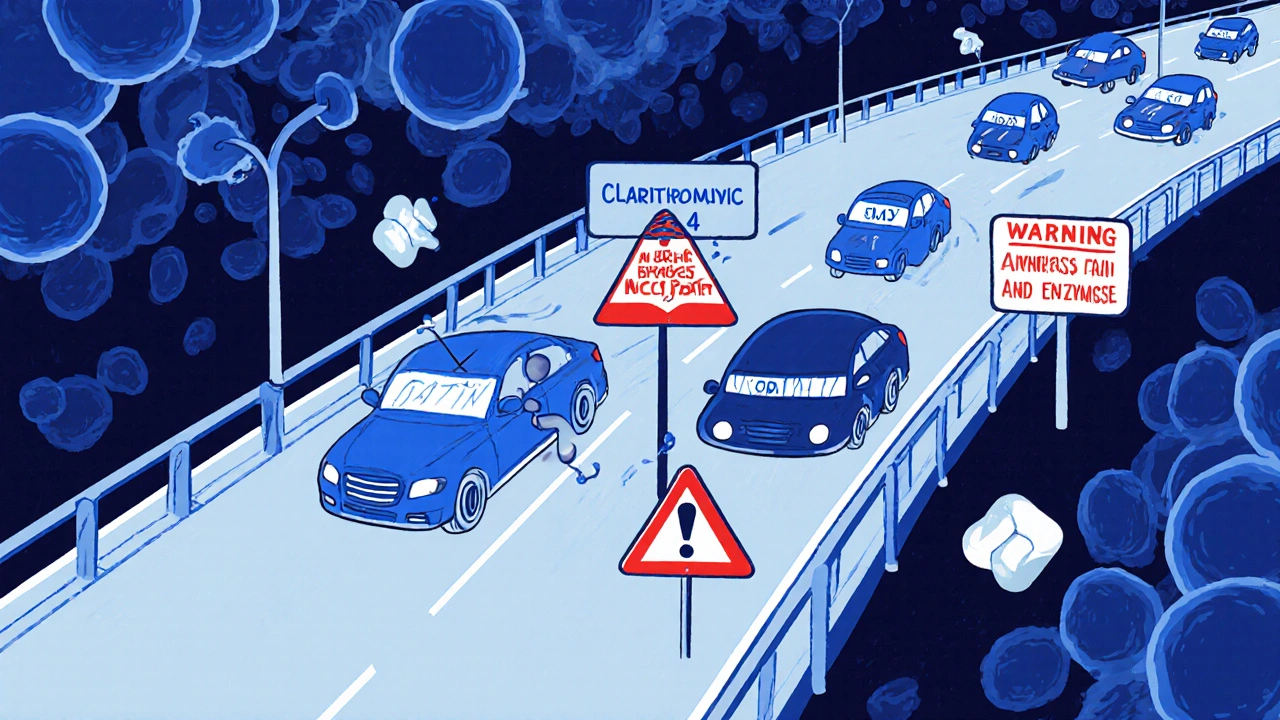
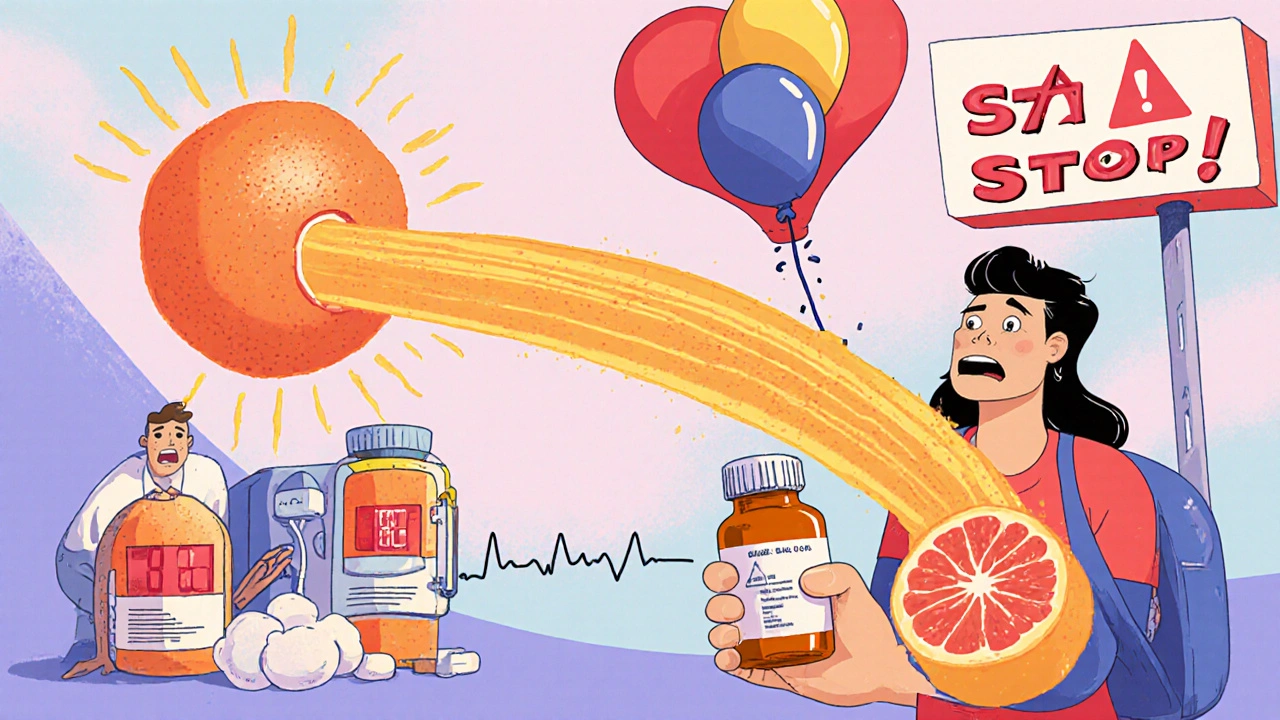
Think of your body like a busy highway. Drugs are cars trying to get through. Some need to be broken down by enzymes-mainly the cytochrome P450 system, especially CYP3A4. This enzyme handles about half of all prescription drugs. Now imagine another drug comes in and slams on the brakes for that enzyme. Suddenly, your statin, your blood thinner, or your antidepressant builds up in your bloodstream like traffic backed up for miles. That’s pharmacokinetic interaction: one drug changes how another is absorbed, metabolized, or cleared. For example, grapefruit juice doesn’t just taste bitter-it shuts down CYP3A4 in your gut. One glass can make felodipine (a blood pressure drug) hit your system at 300% more than it should. The result? Dizziness, swelling, even heart rhythm problems. Then there’s pharmacodynamic interaction-when drugs act on the same target in your body. Warfarin and aspirin both thin the blood. Together, they don’t just add up. They multiply. Studies show the risk of dangerous bleeding jumps by 70-100%. That’s not a small risk. That’s a hospital trip waiting to happen.The Most Dangerous Combinations You Might Not Know About
Some interactions are so risky they’ve pulled drugs off the market. Cisapride, once used for heartburn, was pulled in 2000 after it caused over 80 deaths. Why? It was being taken with antibiotics like clarithromycin, which blocked its breakdown. The result? A deadly heart rhythm called torsades de pointes. The risk? Up to 15 times higher. Here are three high-risk pairs you might be taking right now:- Statin + Clarithromycin: Clarithromycin blocks CYP3A4. Statins like simvastatin build up. Result? Rhabdomyolysis-a muscle breakdown that can fry your kidneys. The risk? 8.4 times higher than with azithromycin (which doesn’t interfere).
- SSRI + Tramadol: Both raise serotonin. Together, they can trigger serotonin syndrome: high fever, seizures, confusion, even death. Over 19 patient reports on Reddit confirm this mix causes real, scary reactions.
- Warfarin + Vitamin K supplements: Warfarin works by blocking vitamin K. If you suddenly start taking a supplement with vitamin K-say, from a green smoothie or multivitamin-your INR plummets. Blood clots form. Stroke risk spikes.
Genetics Play a Bigger Role Than You Think
Two people can take the exact same drugs, at the same doses, and one gets sick while the other feels fine. Why? Genetics. About 3-10% of Caucasians are “poor metabolizers” of CYP2D6. That enzyme turns codeine into morphine. If you’re one of them, codeine doesn’t work. But if you’re an “ultra-rapid metabolizer”? You turn codeine into morphine too fast. One pill can overdose you. The FDA now requires pharmacogenetic warnings on over 30% of commonly prescribed drugs. That’s why some people get terrible side effects from drugs that work fine for others. It’s not bad luck. It’s biology.
Why Doctors Miss These Interactions
You’d think electronic health records would catch every dangerous mix. But they don’t. A 2023 survey of 3,500 doctors found 74% felt overwhelmed by drug interaction alerts. And here’s the kicker: 90-95% of those alerts are ignored. Why? Because most are low-risk noise. Your EHR flags every possible interaction-even ones that are theoretical or harmless. After a while, your doctor stops paying attention. Worse, a 2022 study of 1,200 hospital patients found nurses caught 40% of drug interactions that doctors missed. Why? Nurses see the patient daily. They notice the muscle pain, the confusion, the bruising. Doctors see the chart. And the chart doesn’t always tell the whole story. Patients aren’t always aware either. Many don’t tell their doctor about supplements, over-the-counter meds, or even grapefruit juice. One Reddit user wrote: “I took atorvastatin and ate half a grapefruit every morning. I couldn’t walk without pain. No one asked me about my diet.”How to Protect Yourself
You don’t need to be a pharmacist to avoid dangerous interactions. Here’s what actually works:- Keep a full list of everything you take-prescriptions, supplements, vitamins, herbal teas, even cough syrup. Write it down. Bring it to every appointment.
- Ask your pharmacist when you pick up a new prescription: “Could this interact with anything else I’m taking?” Pharmacists are trained for this. They catch what doctors miss.
- Use a trusted interaction checker. Apps like Medscape or Epocrates let you plug in your meds and get real-time alerts. Don’t rely on Google.
- Know your high-risk drugs. Anticoagulants, antiarrhythmics, antipsychotics, and antidepressants are the most likely to cause trouble. If you’re on one of these, be extra careful.
- Don’t start supplements without asking. “Natural” doesn’t mean safe. St. John’s Wort, garlic pills, ginkgo biloba-all can interfere with meds.
The Bigger Picture: It’s Preventable
The FDA says 30-50% of adverse drug reactions are preventable. Drug interactions make up a big chunk of that. That means thousands of hospital stays, emergency visits, and deaths could be avoided every year. New tools are helping. AI models now predict dangerous combos with 89% accuracy. Pharmacogenetic testing is becoming more common. Hospitals using pharmacist-led medication reviews cut hospitalizations by 23%. But technology alone won’t fix this. You have to be part of the solution. If you’re on multiple meds, you’re at risk. That doesn’t mean stop taking them. It means ask questions. Speak up. Be your own advocate.What to Do If You Think You’re Having an Interaction
If you notice new or worsening side effects after starting a new drug-or even after changing your diet or supplements-don’t wait. Look for these red flags:- Sudden muscle pain or weakness (especially with statins)
- Unexplained bruising or bleeding
- Rapid heartbeat, dizziness, or fainting
- Confusion, agitation, or high fever
- Severe nausea or vomiting
Final Thought: Knowledge Is Your Shield
Medications save lives. But they can also hurt you-if you don’t understand how they play together. Drug interactions aren’t a mystery. They’re a science. And that science is well-documented, measurable, and preventable. You don’t need to memorize every enzyme pathway. You just need to know: When you add something new, something could go wrong. Ask. Check. Double-check. Your body will thank you.Can over-the-counter drugs cause dangerous interactions?
Yes. Even common OTC meds like ibuprofen, aspirin, or antacids can interact. Ibuprofen with blood thinners increases bleeding risk. Antacids with antibiotics like tetracycline can block absorption by up to 90%. Always check with a pharmacist before taking anything new, even if it’s sold without a prescription.
Are herbal supplements safe to take with prescription meds?
No, not without checking. Supplements like St. John’s Wort, garlic, ginkgo, and goldenseal can interfere with how your body processes medications. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and heart meds. Garlic and ginkgo can thin your blood. There’s no regulation on their strength or purity, so the risk is unpredictable.
Does grapefruit juice affect all medications?
No. It mainly affects drugs metabolized by CYP3A4-like some statins (simvastatin, atorvastatin), blood pressure meds (felodipine, nifedipine), and immunosuppressants (cyclosporine). But it doesn’t affect others like amlodipine or pravastatin. Always ask your pharmacist if your specific medication is affected.
Can drug interactions happen with just two medications?
Absolutely. You don’t need five or ten drugs to be at risk. Many dangerous interactions happen with just two. For example, combining warfarin and amiodarone-two common drugs-can triple bleeding risk. Even a single new drug can trigger a reaction if it interferes with how your body handles another.
How often should I review my medications?
At least once a year, or anytime you start, stop, or change a medication-including supplements. If you see a new specialist, bring your full list. Many people take meds prescribed by different doctors without realizing the risks. A full medication review can uncover hidden dangers before they cause harm.
16 Comments
brajagopal debbarma
November 3 2025
So the solution is to stop taking medicine? Or just live in a cave? This whole post is just fear porn for people who think their body is a magic box that only works if they follow a 12-step checklist.
People have been taking pills for 50 years without knowing what CYP3A4 is. Most of us are fine. Stop scaring people with science jargon.
Carly Smith
November 3 2025
I took 3 different meds last week and didn’t die so I guess this whole thing is just a pharmaceutical scam to sell more tests and apps
Also why do you think I care about enzymes I’m not a biologist I just want to not feel like crap
And why is everyone suddenly so scared of grapefruit juice like it’s radioactive
My grandma took warfarin and ate grapefruit every day for 20 years she’s 92 and still walks her dog
Stop overcomplicating things
Kurt Stallings
November 4 2025
Pharmacokinetics is not a lifestyle blog
And no one asked for your 12-step survival guide
The real issue is that medicine has become a religion of compliance
And you’re the priest
Next you’ll tell us to bow before our pill organizer
Angie Creed
November 6 2025
This isn’t about drug interactions - it’s about the complete collapse of medical trust.
Doctors don’t listen. Pharmacies don’t warn. Patients are treated like dumb terminals who just need to swallow the next pill.
And now we’re supposed to memorize enzyme pathways just to stay alive?
It’s not ignorance - it’s systemic betrayal.
They sold us convenience and called it care.
Now we’re left holding the bag of side effects and a 300-page interaction checklist.
Who profits?
Not us.
Never us.
Michael Ferguson
November 6 2025
Let me tell you something - I’m on 11 different medications. I’ve had three ER visits because of ‘side effects’ that no one ever warned me about. I’m not exaggerating. I’m not dramatic. I’m just someone who trusted the system.
My cardiologist prescribed me a beta-blocker. My neurologist gave me an antidepressant. My pain doctor added tramadol. No one asked what else I was taking. No one checked for serotonin syndrome. I ended up in the hospital with a fever of 104, muscle rigidity, and confusion. I thought I was having a stroke.
Turns out it was the combo of SSRI and tramadol. The pharmacist at CVS had it flagged - but I didn’t know to ask her. I thought she just handed out pills.
And now I carry a laminated card with every med, dose, and date. I take a photo of every new script before I leave the pharmacy. I call my pharmacist every time I get a new supplement - even if it’s ‘just turmeric.’
I’m not paranoid. I’m just tired of nearly dying because no one thought to connect the dots.
And yes - grapefruit juice is dangerous. I learned that the hard way when my legs turned to jelly after a single glass. No one told me. Not my doctor. Not my nurse. Not the label.
So I’m telling you now. Don’t be like me. Don’t wait until your kidneys fail or your heart goes haywire. Ask. Always ask. Even if it feels dumb. Even if they roll their eyes. You’re not being annoying - you’re being alive.
Patrick Klepek
November 7 2025
Okay but let’s be real - most of these interactions are avoidable if doctors actually talked to each other.
I’ve got my aunt on warfarin, her GP prescribes her a new antibiotic, her cardiologist doesn’t know, and her pharmacist doesn’t get notified until she’s bleeding out.
It’s not the patient’s fault. It’s the system’s failure.
Also - yes, grapefruit juice is wild. But why is it still sold next to the statins in every pharmacy? Like… someone thought this was a good idea?
And St. John’s Wort? I get it - it’s ‘natural.’ But so is arsenic. Natural doesn’t mean harmless.
Maybe the real solution isn’t more apps or checklists - it’s better communication between providers. And maybe a little less assuming patients are ‘noncompliant’ when they’re just confused.
Caden Little
November 8 2025
Y’all are doing amazing just by reading this and caring enough to ask questions 💪
Here’s the good news - you don’t need to be a genius to stay safe. Just do three things:
1. Keep a list - paper or phone app, doesn’t matter.
2. Ask your pharmacist - they LOVE this question. Seriously.
3. If you feel weird after starting something new - don’t wait. Call someone.
I work in a clinic and I see people every day who are terrified because they think they’re ‘doing it wrong.’ You’re not. You’re doing it RIGHT by paying attention.
And if you’re on statins? Skip the grapefruit. Just swap it for an orange. Same vitamin C, zero risk.
You got this. And you’re not alone.
Sebastian Brice
November 10 2025
Look - I get why people roll their eyes at this stuff. I used to be one of them.
‘Oh great, another ‘don’t take this with that’ list.’
But then my mom had a near-fatal bleed after her doctor added aspirin to her blood thinner. She didn’t even know aspirin was a blood thinner. Thought it was just for headaches.
Turns out, a lot of people don’t.
So yeah - maybe the tone is a little ‘medical pamphlet.’ But the message? Vital.
And if you’re thinking ‘I’m fine’ - you’re not the exception. You’re the lucky one. And that luck won’t last if you keep ignoring the red flags.
Just… ask. Even if it feels silly. Even if they sigh.
It’s not about being paranoid.
It’s about being alive.
Jim Aondongu
November 11 2025
People in America overthink everything
My cousin in Nigeria takes five pills a day and drinks palm wine and never goes to hospital
Why? Because he trusts God and his body
You think enzymes are real or just a western invention to sell apps
Stop being afraid of your own medicine
And why do you think doctors are so busy? Because you keep asking them to explain CYP3A4 like they are your personal tutor
Just take the pill and move on
Michael Schaller
November 12 2025
I didn’t know grapefruit juice could do that until I started feeling like my legs were made of cement. I thought it was just aging. Turns out it was simvastatin + grapefruit. My doctor didn’t ask. My pharmacist didn’t say anything. I only figured it out because I read this exact post on Reddit.
Stopped the grapefruit. Two weeks later, I could walk up stairs again.
So yeah. It’s real.
And yeah. It’s scary.
But it’s fixable if you just pay attention.
Kyle Tampier
November 12 2025
THEY’RE LYING TO YOU. THE PHARMA COMPANIES KNOW THIS. THEY’RE SUPPRESSING THE TRUTH. THE FDA IS IN THEIR POCKET. YOU THINK THEY WANT YOU TO KNOW THAT 70% OF DRUG INTERACTIONS ARE PREDICTABLE? NO. THEY WANT YOU TO BE AFRAID AND KEEP TAKING THE NEXT PRESCRIPTION. THEY’RE MAKING BILLIONS OFF YOUR CONFUSION. AND NOW THEY WANT YOU TO BUY AN APP TO ‘CHECK’ THE DANGERS THEY CREATED. STOP TRUSTING THE SYSTEM. START TRUSTING YOURSELF. AND STOP EATING GRAPES. THEY’RE PROBABLY GENE-EDITED TOO.
Tom Caruana
November 14 2025
I took my blood pressure med and then had a green smoothie with kale and ginger and now I’m pretty sure I’m gonna die 😭
My heart is racing and I can’t breathe and I think the vitamin K is attacking my liver??
Someone please tell me if I’m dying?? I’m crying right now 😭😭😭
I just wanted to be healthy 😭
Is it too late?? Should I go to the ER??
My doctor didn’t say anything about kale 😭
HELP
Muzzafar Magray
November 15 2025
This is why you people are always sick
You think your body is some fragile machine that breaks if you breathe wrong
My father took 14 pills a day for 15 years and never went to hospital
He didn’t know what CYP3A4 was
He didn’t use apps
He just lived
Stop overthinking your meds
And stop blaming doctors for your anxiety
You’re not sick from drugs
You’re sick from fear
Renee Williamson
November 16 2025
Okay but what if the whole thing is a lie? What if the enzymes don’t even exist? What if this is just corporate propaganda to make us buy more tests and apps and supplements to ‘fix’ the problems they created??
I read this whole thing and now I’m terrified of my own skin
What if my coffee is secretly killing me??
What if my multivitamin is a Trojan horse for Big Pharma??
What if the pharmacist is just reading from a script??
What if the FDA is run by robots who hate humans??
I need to go lie down now
Caden Little
November 17 2025
Hey - if you’re panicking about your green smoothie, breathe.
One serving of kale won’t kill you. Vitamin K in food doesn’t usually mess with warfarin unless you’re eating 3 cups a day, every day.
Consistency is key. Not fear.
If you’re on warfarin, just keep your veggie intake steady. No need to quit kale. Just don’t go from zero to hero overnight.
You’re not dying. You’re just scared. And that’s okay.
Call your pharmacist. They’ll tell you exactly what to do. No drama. Just facts.
You got this. 💪






Alexis Hernandez
November 1 2025
Man, I never realized grapefruit juice could turn my statin into a nuclear reactor. I used to eat half a grapefruit every morning like it was a health hack. Turns out I was just playing Russian roulette with my muscles. Thanks for the wake-up call.
Now I check every new pill with my pharmacist like they’re the gatekeeper to my survival. Worth the 5-minute chat.
Also, St. John’s Wort? Yeah, I tried it for ‘low mood.’ Ended up feeling like my brain was on fire and my birth control was useless. Lesson learned.
Doctors don’t ask about supplements. They assume you’re not dumb enough to mix stuff. But we are. We’re all just trying to feel better.
So yeah. Keep the list. Ask the pharmacist. Don’t Google it. Your kidneys will thank you.
And stop drinking grapefruit juice like it’s kombucha. It’s not a superfood. It’s a silent assassin.