Sleep Tracker for Lymphoma Patients
Track Your Sleep for 7 Days
Your Sleep Summary
Total Sleep Time
0 hours
Sleep Efficiency
0%
Average Awakenings
0
Sleep Quality Progress
Personalized Recommendations
Track your sleep for 7 days to receive personalized recommendations.
- Review your sleep log with your oncology nurse or palliative care team.
- Consider implementing consistent sleep hygiene practices.
When a diagnosis of Lymphoma a group of blood cancers that originate in the lymphatic system lands on your doorstep, the list of worries can feel endless. One problem that often slips under the radar is sleep - you might find yourself tossing and turning even before treatment starts. If you’ve ever asked, “Why can’t I fall asleep when everything else feels so chaotic?” you’re not alone. Below is a practical guide that turns sleepless nights into a manageable part of the cancer journey.
Why Sleep Gets Disrupted in Lymphoma
Understanding the why helps you target the how. Several factors converge to steal your shut‑eye:
- Treatment side‑effects: Chemotherapy the use of drugs to kill fast‑growing cancer cells can cause nausea, hot flashes, and neuropathy that flare up at night.
- Medications: Corticosteroids steroids often prescribed to reduce inflammation and control swelling are notorious for boosting energy and stirring up anxiety.
- Emotional load: Anxiety and Depression common mood disorders that affect sleep patterns can keep the mind buzzing.
- Pain and restless legs: Bone pain or Restless Leg Syndrome an urge to move the legs, especially at rest make it hard to settle.
- Hospital environment: Bright lights, nightly vitals checks, and unfamiliar noises turn a bedroom into a clinic.
All of these add up to what clinicians call Sleep Disturbance any interruption of normal sleep architecture, including difficulty falling asleep, staying asleep, or waking too early. When sleep is fragmented, fatigue spikes, immune function dips, and treatment tolerance drops. In short, good sleep isn’t a luxury - it’s a part of the therapy.
How to Spot Insomnia Early
Insomnia is the most common form of sleep disturbance in cancer patients. If you answer “yes” to any of the following, it’s time to act:
- Do you spend more than 30 minutes lying awake each night?
- Do you wake up two or more times and have trouble falling back asleep?
- Do you feel unrested even after a full night in bed?
- Are you relying on caffeine, nicotine, or daytime naps to get through the day?
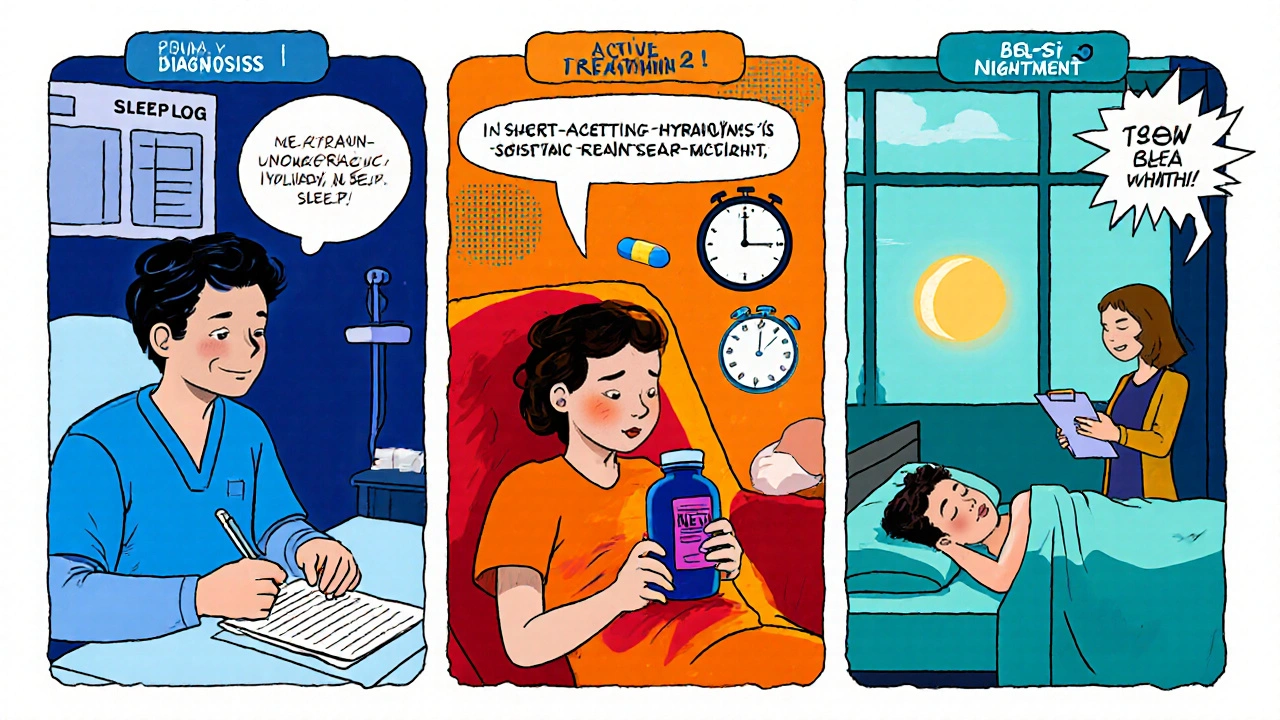
Keep a simple sleep log for a week - note bedtime, wake‑time, nighttime awakenings, and any medication taken after 6pm. This log becomes a powerful conversation starter with your oncology nurse or palliative‑care team.
Non‑Pharmacologic Strategies that Work
Before reaching for a pill, try these evidence‑based tactics. They’re low‑cost, have no side‑effects, and many patients notice improvement within a few nights.
- Sleep Hygiene: Keep the bedroom cool (18‑20°C), dark, and quiet. Reserve the bed for sleep and intimacy only - no scrolling on your phone.
- Scheduled Wind‑Down: Start a calming routine 30‑45minutes before bed - dim the lights, sip a warm (caffeine‑free) tea, do gentle stretches.
- Limit Daytime Naps: If you must nap, keep it under 20minutes and before 2pm.
- Mind‑Body Practices: Deep‑breathing, guided imagery, or a short meditation can lower cortisol, the stress hormone that keeps you alert.
When these basics aren’t enough, consider Cognitive Behavioral Therapy for Insomnia a structured, short‑term program that changes thoughts and behaviors around sleep (CBT‑I). Numerous studies show CBT‑I improves sleep efficiency by 15‑20% in cancer patients, often without any medication.
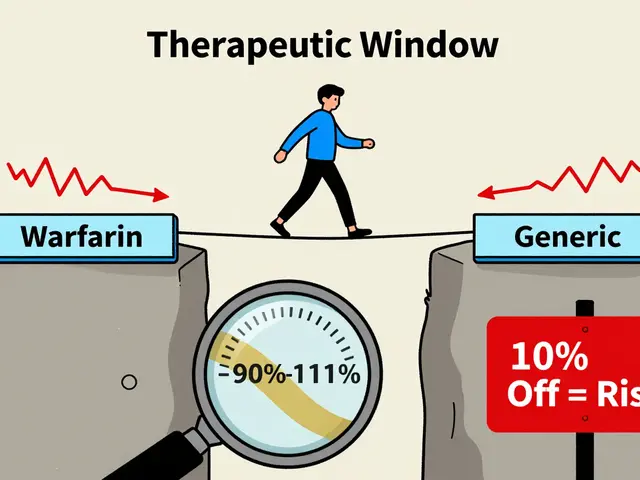
When Medication Becomes Necessary
Pharmacologic help is perfectly fine when non‑drug methods fall short, especially if you’re battling severe anxiety or pain. Below is a quick comparison of the most commonly prescribed sleep aids alongside natural options.
| Option | Type | Typical Dose / Use | Onset (minutes) | Pros | Cons |
|---|---|---|---|---|---|
| Zolpidem | Prescription hypnotic | 5‑10mg at bedtime | 15‑30 | Fast sleep onset, short half‑life | Risk of dependence, daytime drowsiness |
| Temazepam | Benzodiazepine | 7.5‑15mg at bedtime | 30‑45 | Effective for anxiety‑related insomnia | Potential tolerance, falls risk in older adults |
| Melatonin | Endogenous hormone supplement | 0.5‑5mg 30min before bed | 30‑60 | Very low side‑effect profile, supports circadian rhythm | Variable over‑the‑counter quality |
| CBT‑I | Behavioral therapy | 6‑8 weekly sessions | Variable (effects seen after 2‑3 weeks) | Long‑term benefit, no medication | Requires trained therapist, time commitment |
| Sleep Hygiene | Lifestyle bundle | Daily practice | Variable | Zero cost, improves overall health | Needs consistency and patience |
Talk with your oncologist before starting any new pill. Some sleep medications can interact with chemotherapy agents or worsen nausea.
Tailoring a Sleep Plan for Your Treatment Phase
Sleep needs shift from diagnosis to remission. Here’s a quick guide for each stage:
- Diagnosis & Initial Work‑up: Focus on sleep hygiene, limit caffeine, start a sleep log.
- Active Treatment (chemo/radiation): Add melatonin if night‑time hot flashes are an issue; consider short‑acting hypnotics for breakthrough insomnia; schedule CBT‑I early if possible.
- Post‑Treatment / Surveillance: Gradually taper any hypnotics; continue CBT‑I or mindfulness; address lingering fatigue with daytime activity pacing.
Remember, lymphoma sleep disturbances can also be a sign that your treatment dose needs adjusting. Never assume it’s “just stress” - bring the data from your sleep log to the clinic.
Common Pitfalls and How to Avoid Them
Even with a solid plan, missteps happen. Spot these early:
- Over‑reliance on caffeine: A single cup after lunch is fine, but a late‑day latte spikes cortisol.
- Screen time in bed: Blue light suppresses melatonin; use night‑mode or read a paper book instead.
- Skipping meals: Low blood sugar can trigger nighttime awakenings.
- Ignoring pain medication timing: Take prescribed pain meds at regular intervals rather than waiting for pain to flare.
- Self‑prescribing over‑the‑counter sleep aids: They may contain antihistamines that worsen dryness or interact with other drugs.
Next Steps & Troubleshooting
If you’ve tried the basics and still feel exhausted, follow this checklist:
- Review your sleep log with a nurse - look for patterns.
- Ask about a low‑dose melatonin regimen; note the brand and dosage.
- Request a referral to a psychologist trained in CBT‑I.
- Evaluate nighttime pain - adjust analgesic schedule if needed.
- Consider a brief trial of a prescription hypnotic for no more than 2‑4 weeks, then taper.
Each step should be documented so you can see what works and what doesn’t. If insomnia persists despite these measures, a sleep study may uncover hidden sleep apnea or periodic limb movement disorder, both treatable with CPAP or medication.
Frequently Asked Questions
Can melatonin interfere with chemotherapy?
Current research shows melatonin does not reduce the effectiveness of standard chemo agents. In fact, some trials suggest it may protect healthy cells and improve quality of life. Always discuss dosage with your oncologist.
Is it safe to use over‑the‑counter antihistamine sleep aids?
Antihistamines can cause dry mouth, constipation, and next‑day grogginess, which may worsen chemotherapy side‑effects. They’re best reserved for occasional use and only after checking with your care team.
How long does CBT‑I usually take to show results?
Most patients notice a measurable improvement after 2‑3 sessions, with full benefits emerging around 6‑8 weeks. The key is consistent practice of the sleep‑restriction and stimulus‑control techniques taught in the program.
What if I’m already on a high dose of steroids?
Steroids can trigger vivid dreams and insomnia. Talk to your doctor about tapering the dose or switching to a steroid‑sparing regimen. Adding melatonin or low‑dose trazodone can also counteract the stimulant effect.
Should I avoid napping completely?
A brief 20‑minute nap can recharge you without hurting nighttime sleep, especially if you’re dealing with treatment‑related fatigue. Keep it early in the day and set an alarm.
14 Comments
Rhys Black
October 19 2025
It’s almost tragic how the very disease that threatens our bodies also hijacks the sanctity of night. The flickering hospital lights become a cruel reminder that rest is a luxury. You’re battling not just malignant cells but the insidious creep of insomnia that gnaws at your resolve. While the medical team charts chemo protocols, they often sideline the quiet misery of sleeplessness. Recognizing this hidden foe is the first act of rebellion against the tyranny of cancer. So, arm yourself with the tools above and refuse to surrender your nights. Begin with a consistent sleep‑hygiene routine that signals to your brain the end of day. Keep the bedroom cool, dark, and free of electronic glare. A brief wind‑down period-perhaps a warm tea and gentle stretches-can lower cortisol. Track your sleep patterns in a log; data is a powerful ally in your conversations with clinicians. If pain spikes in the early hours, discuss adjusting analgesic timing with your pain specialist. Consider melatonin supplementation after consulting your oncologist, especially if night‑time hot flashes disturb you. When non‑pharmacologic measures fall short, a short‑acting hypnotic may bridge the gap temporarily. However, always aim to taper off medications to avoid dependence and daytime grogginess. Ultimately, combing these strategies creates a personalized plan that restores the restorative power of sleep.
Tom Lane
October 23 2025
Let’s keep it practical-start a simple sleep log tomorrow night and jot down when you actually fall asleep, not when you *think* you should. Pair that with a cool, dark bedroom and a screen‑free half hour before lights‑out. You’ll be surprised how much patterns emerge by just tracking. If you notice pain spikes at 2 a.m., bring that up at your next oncology visit; there’s often a tweak you can make. Small, consistent steps beat grand, sporadic attempts every time.
Mike Rylance
October 27 2025
From a clinical perspective, it is essential to differentiate between transient sleep disruption due to acute stress and chronic insomnia that may impede treatment efficacy. Evidence indicates that untreated insomnia can exacerbate fatigue, diminish immune response, and reduce tolerance to chemotherapy. Therefore, incorporating validated tools such as the Insomnia Severity Index into routine assessments is advisable. Collaboration between oncology, nursing, and palliative care teams ensures a comprehensive approach.
Srinivasa Kadiyala
October 31 2025
Actually-let’s pause-most of the “standard” sleep‑hygiene tips are just common‑sense, and they rarely address the underlying neurochemical chaos induced by steroids!!!; you could argue that focusing on melatonin supplements is a more direct way to re‑establish circadian rhythm; yet, the literature is still split, and many clinicians overprescribe hypnotics without proper taper plans.
Alex LaMere
November 4 2025
Sleep‑related side effects of chemotherapy are dose‑dependent; monitor them closely. Avoid self‑medicating with antihistamines; they interact with anti‑emetics. Document everything; bring the log to your clinician.
KayLee Voir
November 8 2025
I’ve seen many patients find comfort in a gentle wind‑down routine-perhaps a warm, caffeine‑free tea and a few minutes of guided breathing. It’s not a cure‑all, but it signals to your brain that it’s time to shift gears. Also, remember that it’s okay to ask for help; a simple conversation with your nurse can lead to adjustments in pain meds that make a night’s sleep possible.
Matt Cress
November 12 2025
Sure, because nothing says "relax" like a fluorescent hallway at 3 am-totally zen, right? Maybe try earplugs, or just embrace the industrial chic vibe of the oncology floor.
Paige Crippen
November 16 2025
Don’t forget that the pharma industry pushes sleep meds to keep you dependent while they profit from your chronic fatigue. Keep an eye on what they’re really selling you.
sweta siddu
November 20 2025
Thanks for the tip, KayLee! I actually tried a short yoga flow before bed and it helped calm my mind. I also use a lavender diffuser-some patients swear by the scent for deeper sleep. 😊
Ted Mann
November 24 2025
Alex, your point about documentation is spot on-recording data turns subjective misery into objective evidence. Think of it as a personal scientific experiment where you adjust variables like melatonin dosage and measure outcomes. This systematic approach not only empowers you but also provides clinicians with concrete data to fine‑tune therapy.
Brennan Loveless
November 29 2025
Rhys, while the drama is vivid, let’s not overlook that many of these “nighttime battles” are amplified by anxiety that could be mitigated with cognitive techniques rather than just medications. CBT‑I, for instance, restructures the narrative you tell yourself about cancer and sleep, reducing the emotional weight you described.
Vani Prasanth
December 3 2025
Sweta, happy to hear the yoga worked! Adding a brief mindfulness meditation-just five minutes focusing on breath-can further enhance the calm you’re seeking. Consistency is key; make it a nightly ritual and you’ll likely see cumulative improvement over weeks.
Maggie Hewitt
December 7 2025
Oh sure, because if you just “stop scrolling” at 2 a.m. the universe will magically grant you eight perfect hours of REM-no, that’s not how it works. The reality is that our bodies need cues, and sometimes the hospital environment is the worst cue of all. Invest in a good pair of blackout curtains, white‑noise app, and maybe a funny audiobook to distract the mind. If that still fails, remember that a short, intentional nap isn’t cheating-it’s strategic recovery.





Brian Lancaster-Mayzure
October 15 2025
Hang in there-you’re not alone in this sleep battle.