
Heat & Cold Therapy Selector
Heat and Cold Therapy is a combined approach that uses temperature extremes to relieve muscle stiffness. It blends thermotherapy (warming) and cryotherapy (cooling) to improve blood flow, reduce inflammation, and calm painful trigger points. When applied correctly, the technique can speed up recovery from everyday aches, sports injuries, and chronic tightness.
What Causes Muscle Stiffness?
Muscle stiffness is a state of reduced flexibility that often follows over‑use, poor posture, or sudden strain. The underlying mechanisms include micro‑tears in muscle fibers, accumulation of lactic acid, and tight fascia limiting range of motion. Studies from the British Institute of Sports Medicine (2023) show that up to 65% of office workers report stiffness in the neck and shoulders after a full day at a desk.
Heat Therapy: How It Works
Heat therapy is a form of thermotherapy that delivers temperatures between 38°C and 45°C (100°F‑113°F) to the affected area. The warmth dilates blood vessels, boosting circulation and delivering oxygen‑rich blood to damaged tissues. This process accelerates the removal of metabolic waste, relaxes tight muscles, and triggers the release of endorphins, providing a natural analgesic effect.
- Typical temperature range: 38‑45°C (100‑113°F)
- Preferred devices: electric heating pads, hot water bottles, microwavable gel packs
- Optimal duration: 15‑20 minutes per session, up to three times daily
Cold Therapy: How It Works
Cold therapy is a type of cryotherapy that applies temperatures from 0°C to 15°C (32°F‑59°F). The chill constricts blood vessels, reducing swelling and numbing pain‑signals. It also slows the metabolic rate of injured cells, limiting secondary damage after an acute strain.
- Typical temperature range: 0‑15°C (32‑59°F)
- Preferred devices: reusable ice packs, frozen peas, cold‑gel wraps
- Optimal duration: 10‑15 minutes per session, up to three times daily
When to Choose Heat vs. Cold
The decision hinges on the injury phase and the goal of treatment. Use heat therapy for chronic tightness, muscle spasm, or to prepare muscles before activity. Choose cold therapy for acute inflammation, recent bruises, or after intense workouts when swelling is present.
| Attribute | Heat Therapy | Cold Therapy |
|---|---|---|
| Temperature Range | 38‑45°C (100‑113°F) | 0‑15°C (32‑59°F) |
| Primary Benefit | Increases blood flow, relaxes muscles | Reduces swelling, numbs pain |
| Best For | Chronic stiffness, pre‑exercise warm‑up | Acute injuries, post‑exercise recovery |
| Typical Duration | 15‑20 min per session | 10‑15 min per session |
| Contraindications | Open wounds, severe dermatitis | Raynaud’s disease, poor circulation |

Step‑by‑Step Guide: Applying Heat Therapy
- Identify the stiff area and clean the skin.
- Choose a heating device (electric pad, hot water bottle, or microwave‑able gel pack).
- Set the temperature to a comfortable warm level; avoid exceeding 45°C to prevent burns.
- Place a thin towel between the device and skin to protect the epidermis.
- Leave on for 15‑20 minutes, then remove and gently stretch the muscle.
- Repeat up to three times daily, especially before activity or during the evening.
Tracking results in a simple log (date, duration, perceived tightness) helps you notice patterns and adjust frequency.
Step‑by‑Step Guide: Applying Cold Therapy
- Wrap the ice pack or frozen peas in a thin cloth; never apply ice directly to skin.
- Position the pack on the stiff or inflamed area.
- Set a timer for 10‑15 minutes; keep the skin visible to avoid frostbite.
- After removal, gently massage the area to encourage blood flow back to normal.
- Rest for at least 30 minutes before re‑applying if needed.
- Use up to three sessions per day during the first 48‑72 hours after an acute flare‑up.
Cold therapy works best when paired with light movement, such as walking or low‑intensity cycling, to prevent stiffness from worsening.
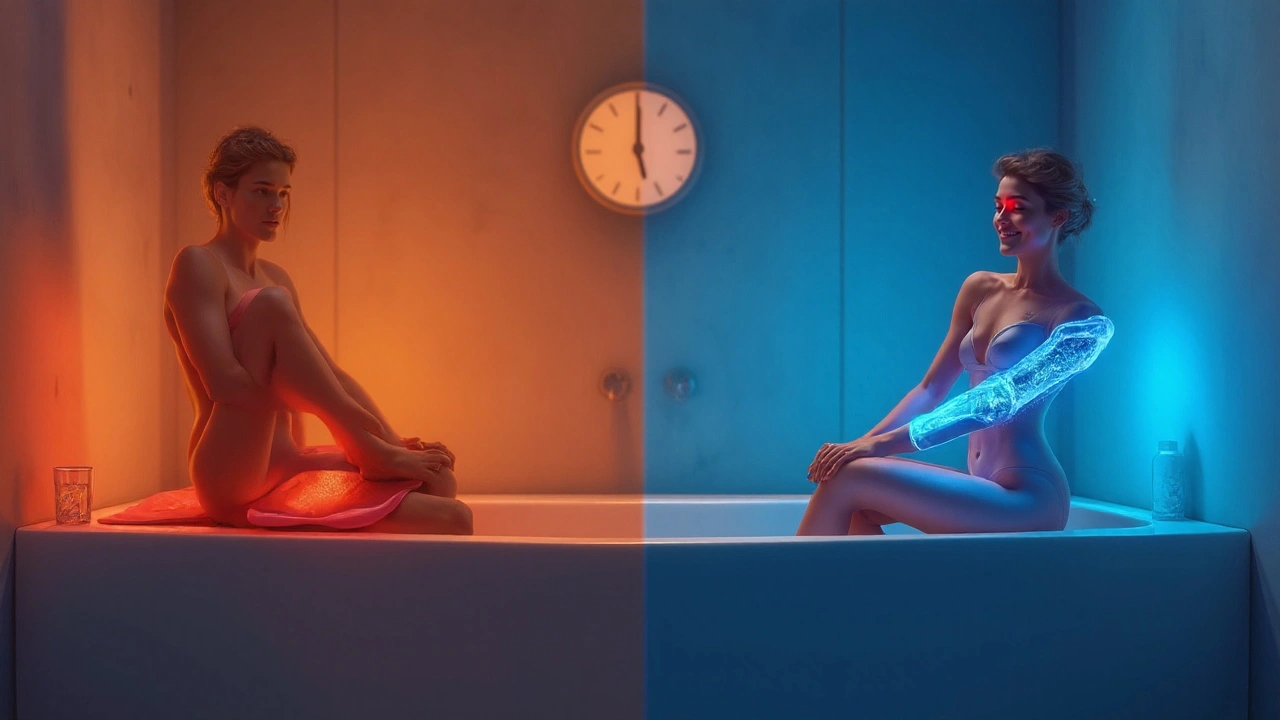
Contrast Therapy: Combining Heat and Cold
Contrast therapy is a technique that alternates heat and cold to create a pumping effect in the circulatory system. The rapid shift between vasodilation and vasoconstriction helps flush metabolic waste and deliver fresh nutrients.
- Start with 3 minutes of heat.
- Switch to 1 minute of cold.
- Repeat the cycle 3‑4 times, finishing with cold for a soothing end.
- Whole session should not exceed 20 minutes.
Athletes often use contrast therapy after intense training sessions; physiotherapists recommend it for chronic back pain when standard heat or cold alone provides limited relief.
Safety Tips & Contraindications
Even simple temperature treatments can backfire if you ignore warning signs.
- Do not apply heat over open cuts, burns, or areas with reduced sensation (e.g., diabetic neuropathy).
- Avoid cold on skin with circulation disorders, such as Raynaud’s phenomenon or severe eczema.
- Limit each session to the recommended time; prolonged exposure can cause skin irritation or tissue damage.
- Pregnant women should consult a healthcare professional before using heat on the abdomen.
- If pain worsens after treatment, discontinue use and seek medical advice.
Related Concepts and Next Steps
Understanding the broader context can make your therapy more effective. Below are key concepts that often intersect with heat and cold therapy.
- Physiotherapy - professional guided exercises that complement temperature treatment.
- Fascia release - manual techniques that target the connective tissue surrounding muscles.
- Trigger point therapy - focused pressure to deactivate tight knots.
- Stretching routines - dynamic and static stretches that maintain flexibility after heat.
- Inflammation markers - blood tests (CRP, ESR) that help gauge the severity of acute swelling.
After mastering heat and cold therapy, you might explore "How to Create a Home Physiotherapy Kit" or "Effective Stretching Sequences for Office Workers"-both natural extensions of today’s topic.
Frequently Asked Questions
Can I use both heat and cold on the same day?
Yes, you can alternate them if you follow the contrast therapy protocol: start with heat, switch to cold, and repeat. Avoid applying them back‑to‑back without a short break, as the sudden temperature shift can shock the skin.
How often should I repeat a heat or cold session?
For chronic stiffness, three heat sessions per day work well. For acute inflammation, limit cold therapy to three 10‑minute bouts daily, especially during the first 48 hours.
Is there a risk of burning with heat packs?
Burns can occur if the temperature exceeds 45°C or if the pack sits on the skin for longer than 20 minutes. Always use a thin towel barrier and check the skin temperature after each session.
What if I have poor circulation-should I avoid cold therapy?
People with peripheral vascular disease, Raynaud’s, or diabetes‑related neuropathy should consult a doctor before using cold packs, as reduced blood flow can increase the risk of tissue damage.
Can heat therapy help after a marathon?
Yes, applying gentle heat 24‑48 hours post‑race can relieve lingering muscle tightness, but it should be combined with light stretching and hydration to avoid lingering inflammation.
Do I need special equipment for contrast therapy at home?
No fancy gear is required-just a reliable heating pad and a reusable ice pack. The key is timing; use a kitchen timer or phone alarm to keep each phase within the recommended minutes.
6 Comments
Lauren Carlton
September 24 2025
The article’s misuse of the word “its” versus “it’s” undermines its credibility.
Katelyn Johnson
September 24 2025
I love how this guide makes everyone feel included and supported it’s a great resource for people from all backgrounds and fitness levels remember to listen to your body and adjust the temperature if it feels too intense keep sharing your experiences and we can all learn together
Elaine Curry
September 24 2025
Hey, I’m not a doctor but I’ve tried the contrast method after my marathon and it actually helped me bounce back faster maybe you should try it too even if you’re just a weekend warrior go ahead and give it a shot
Patrick Fortunato
September 24 2025
Honestly these therapies are all the rage in my country where we’ve been using hot stone treatments for centuries it’s just common sense to warm up those sore muscles before a big game and we never bother with all the fancy gadgets just a simple hot water bottle does the trick
Manisha Deb Roy
September 24 2025
Pro tip: always wrap the ice pack in a thin towel to avoid frostbite and use a timer so you don’t overdo it. Also, a quick stretch after a heat session can really lock in the looseness. definetly try this combo for best results.





Kaustubh Panat
September 24 2025
The nuanced interplay between thermodynamic principles and human physiology is often underappreciated by the lay public. Heat therapy, when executed with methodological precision, engenders vasodilation that facilitates metabolic clearance of nociceptive mediators. Conversely, cold therapy precipitates vasoconstriction, thereby attenuating the inflammatory cascade. It is imperative to calibrate temperature gradients within the therapeutic window of 38‑45 °C for heat and 0‑15 °C for cold to avert iatrogenic injury. A judicious practitioner will also consider tissue perfusion status before initiating any modality. The temporal sequencing of applications-whether singular or contrastive-bears significant ramifications for cellular homeostasis. Empirical studies from elite sports medicine institutions corroborate that contrast therapy amplifies lymphatic return more effectively than monotherapy. Moreover, the integration of active mobilization between thermal episodes optimizes neuromuscular re‑education. One must not overlook the contraindications; open wounds, severe dermatitis, Raynaud’s phenomenon, and diabetic neuropathy preclude indiscriminate use. The recommended duration of 15‑20 minutes for heat and 10‑15 minutes for cold is not arbitrary but rooted in thermodynamic equilibrium concepts. Exceeding these intervals invites thermal burns or frostbite, respectively. When disseminating this knowledge, it is essential to employ vernacular that respects the intellectual rigor of the discipline. Practitioners should also maintain meticulous logs, noting temperature, duration, and subjective pain scores. Such documentation empowers evidence‑based adjustments and fosters longitudinal outcome tracking. Finally, the ethical obligation to advise patients of potential adverse effects cannot be overstated, lest we devolve into quacks exploiting thermal gimmicks.