
Chronic pancreatitis isn’t just a diagnosis-it’s a daily battle. For many, it means waking up with pain that doesn’t fade, meals that feel like a gamble, and a medicine cabinet full of pills that don’t always work. Unlike acute pancreatitis, which comes on suddenly and often resolves, chronic pancreatitis is a slow, relentless breakdown of the pancreas. The organ that once helped digest food and regulate blood sugar now struggles to do either. And the biggest challenge? Chronic pancreatitis pain doesn’t respond like typical pain. It’s not just inflammation. It’s nerve damage. It’s scarring. It’s a system that’s broken from the inside out.
Pain That Won’t Quit
Eight out of ten people with chronic pancreatitis live with constant or recurring abdominal pain. It’s not the sharp, stabbing kind you get from food poisoning. It’s deeper-a dull, burning ache that radiates to your back. Some describe it as a band tightening around their midsection. Others say it feels like someone is twisting their insides. This pain doesn’t go away with rest or over-the-counter meds. It lingers for weeks, months, even years.
Doctors start with the WHO pain ladder. That means beginning with simple painkillers. Acetaminophen (paracetamol) is usually the first step. Up to 4,000 mg a day is safe for most, and for some, it brings relief. But if that doesn’t cut it, the next step isn’t stronger opioids-it’s nerve-targeting drugs. Gabapentin and pregabalin, originally for seizures and nerve pain, are now standard. Many patients find 1,800-3,600 mg of gabapentin daily reduces their pain by nearly half. Amitriptyline, an old-school antidepressant, works surprisingly well too. It’s not about mood-it’s about calming overactive pain nerves.
When those fail, tramadol becomes the go-to opioid. It’s less addictive than morphine, and studies show it’s the most effective oral opioid for this condition. But it’s not perfect. About one in four people get nausea or constipation. And even then, it doesn’t work for everyone. That’s why specialists avoid jumping to strong opioids like oxycodone unless absolutely necessary. The risk of dependence is real. About 30% of patients eventually need stronger pain control, but only after trying everything else.
Enzyme Therapy: More Than Just Pills
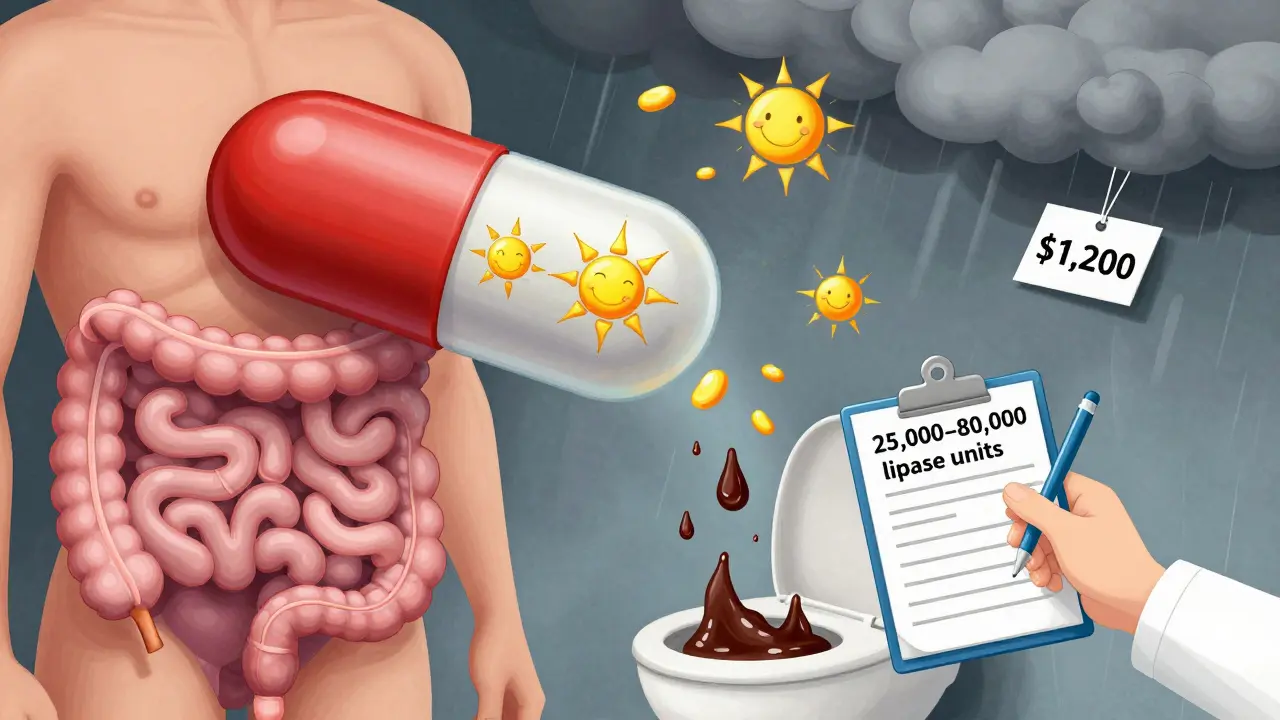
When the pancreas can’t make digestive enzymes, food doesn’t break down. Fat slips through undigested, causing greasy, foul-smelling stools. Weight loss follows. Nutrients vanish. That’s where pancreatic enzyme replacement therapy (PERT) comes in.
You don’t just take these pills-you time them. They must be swallowed right before or with your first bite. If you take them too early or too late, they won’t work. Doses range from 25,000 to 80,000 lipase units per meal. For a large dinner with steak and fries, you might need six to eight capsules. That’s a lot of pills. Many patients give up because of the burden.
Not all enzymes are the same. Brands like Creon, Zenpep, and Pancreaze are enteric-coated, meaning they survive stomach acid and release in the small intestine. But if you’re on a non-enteric coated version, you’ll need a proton pump inhibitor like omeprazole to protect them. Studies show high-dose PERT can reduce pain in nearly half of patients-not because it fixes the pancreas, but because undigested fat irritates the gut and triggers pain signals. When fat is absorbed properly, that irritation drops.
Still, effectiveness drops as the disease progresses. In early stages, PERT helps 60-70% of people. In advanced cases, that falls to 30-40%. And cost is a barrier. Monthly prices can hit $1,200. Insurance often fights coverage. Many patients skip doses or cut them in half just to make it last.
Nutrition: What to Eat, What to Avoid
For years, doctors told chronic pancreatitis patients to go low-fat. Eat lean chicken, skip oils, avoid dairy. But the evidence isn’t as clear as it seems. Yes, high-fat meals can trigger pain in 60-70% of patients. But forcing extreme fat restriction doesn’t always help-and it can make malnutrition worse.
Medium-chain triglycerides (MCTs) are the secret weapon. Unlike regular fats, MCTs don’t need pancreatic enzymes to be absorbed. They go straight from your gut into your bloodstream. That’s why formulas like Peptamen are used in clinics. One study found patients drinking three cans a day of an MCT-based shake cut their pain by 30% in just ten weeks. You can find MCT oil in health stores. Add a tablespoon to smoothies or soups. It’s tasteless and easy.
Antioxidants also play a role. A daily mix of selenium, vitamin C, vitamin E, beta-carotene, and methionine reduced pain in over half of patients in a major trial. These aren’t magic bullets, but they reduce oxidative stress in the pancreas, which may slow damage. Many patients report feeling more energy after starting them.
And then there’s the big one: alcohol. Even if you’ve already quit, it’s worth repeating-complete abstinence improves pain control in 40-50% of people within six months. Tobacco is just as bad. Smokers with chronic pancreatitis have two to three times the risk of worsening disease. Quitting isn’t just advice-it’s survival.
When the Pills Don’t Work
Some patients reach a point where nothing helps. That’s when interventions come in. One option is a celiac plexus block. A needle is guided near the nerves that carry pain signals from the pancreas. Alcohol or steroids are injected to deaden them. For many, it brings relief for three to six months. One patient in Alberta described it as “nine months of peace after two years of agony.”
Endoscopic procedures like ERCP can open blocked pancreatic ducts. A stent is placed to drain fluid and reduce pressure. About 60-70% get relief at first, but nearly half see pain return within a year.
Surgery is the last resort-but it can be life-changing. The Frey procedure removes part of the pancreas and opens the duct. About 70-80% of patients have lasting pain relief five years later. Then there’s TPIAT-total pancreatectomy with islet autotransplantation. The whole pancreas is removed, but insulin-producing cells are harvested and reinfused into the liver. It’s radical. You’ll need lifelong insulin. But 85-90% of patients become pain-free. For those trapped in a cycle of opioids and hospital visits, it’s not a last resort-it’s a second chance.
The Hidden Struggle
Behind the medical facts are real people. On patient forums, 65% say their pain isn’t controlled. One Reddit user tried eight different meds before gabapentin and tramadol finally worked. Others quit enzymes because they couldn’t afford them. Many say they waited two to three years just to get diagnosed.
And then there’s the loneliness. Chronic pain wears you down. Sleep disappears. Work becomes impossible. Relationships strain. Yoga, once dismissed as alternative, is now backed by science. A University of Pittsburgh study found biweekly yoga sessions improved quality of life by 35% over 12 weeks. Breathing, stretching, mindfulness-it’s not a cure, but it’s a tool.
Doctors are starting to treat this as a whole-person condition. Pain specialists, dietitians, addiction counselors, and mental health providers now work together. But only 25% of community hospitals have these teams. Most patients are left to navigate it alone.
What’s Next?
The future is coming. A new enzyme formulation called LipiGesic™, with smarter pH-based release, is showing 20% better fat absorption in trials. The NIH has poured $15 million into finding better pain treatments. And researchers are looking at genetic markers to predict who will get worse pain-and when.
One thing’s clear: chronic pancreatitis isn’t going away. But with the right mix of enzymes, nutrition, pain control, and support, many can live better. It’s not about fixing the pancreas. It’s about living with it-without being ruled by it.
8 Comments
Mike Berrange
January 16 2026
Let me just say-this article is technically accurate, but it completely ignores the systemic failure of the U.S. healthcare system. You mention $1,200/month for enzymes? That’s criminal. Insurance companies treat this like a luxury, not a medical necessity. And the fact that you have to time pills to the second? That’s not management-that’s a full-time job with no paycheck.
Dan Mack
January 17 2026
They don’t want you to know this, but pancreatitis is tied to GMOs and fluoride in the water. Big Pharma doesn’t want you to heal naturally-they want you hooked on gabapentin and Creon. The real cure? Cold laser therapy and liver cleanses. I’ve seen it work. The doctors won’t tell you because they’re paid by the drug companies.
And yes, I’ve had it for 14 years. I know what’s really going on.
Amy Vickberg
January 18 2026
I was diagnosed three years ago and thought I was done. Then I started taking selenium and vitamin E daily. I didn’t expect much, but my energy came back. Not a miracle, but a real shift. And I started eating small meals with MCT oil-no more greasy stools. It’s not glamorous, but it’s something. You’re not alone in this. Keep going.
And if you can’t afford enzymes, reach out to patient groups. Someone will help you.
Ayush Pareek
January 20 2026
Hey, I’ve been where you are. Took me two years to get diagnosed too. I used to think I was just ‘eating wrong.’ Turns out, my pancreas was dying. PERT was a nightmare at first-eight pills before every meal? No way.
But I started with half-doses and worked up. Now I use a pill organizer with alarms. It’s dumb, but it works. And MCT oil in my morning coffee? Game changer. You don’t have to do it all at once. One step. One day. One capsule. You got this.
Nishant Garg
January 21 2026
In India, we call this ‘aata ka dard’-the pain of the dough. Your body kneads itself into agony. No one talks about how it steals your joy, not just your digestion. I lost my job because I couldn’t sit through meetings. My wife cried when I couldn’t eat the biryani she spent hours making.
But here’s what no one says: the enzymes? They’re not just pills. They’re dignity. You take them not because you’re weak, but because you’re still fighting. And that’s worth more than any opioid.
Nicholas Urmaza
January 22 2026
Stop treating this like a diet issue. This is a neurological disaster with a digestive side effect. The WHO ladder is a joke when your nerves are on fire. Gabapentin works because it doesn’t care about your pancreas-it shuts down the alarm. And if you’re still on acetaminophen after six months, you’re not being careful, you’re being reckless.
Get off the fence. Get help. Now.
Sarah Mailloux
January 24 2026
I tried the yoga. Didn’t cure me. But I slept through the night for the first time in a year. That’s not nothing.
And if you’re skipping enzymes because of cost? I’ve been there. Join a Facebook group. Someone will send you a sample. You’re not a burden. You’re a warrior.






Arjun Seth
January 15 2026
Everyone thinks they know what chronic pain is until it's their gut screaming at 3 AM. You take the pills, you count the capsules, you drink the MCT oil like it's holy water-and still, you're just surviving. This isn't a lifestyle choice, it's a prison with a diagnosis.
And no, yoga won't fix your pancreas. Stop pretending it will.