Probiotics with Antibiotics: What Works, What Doesn't, and How to Use Them Right
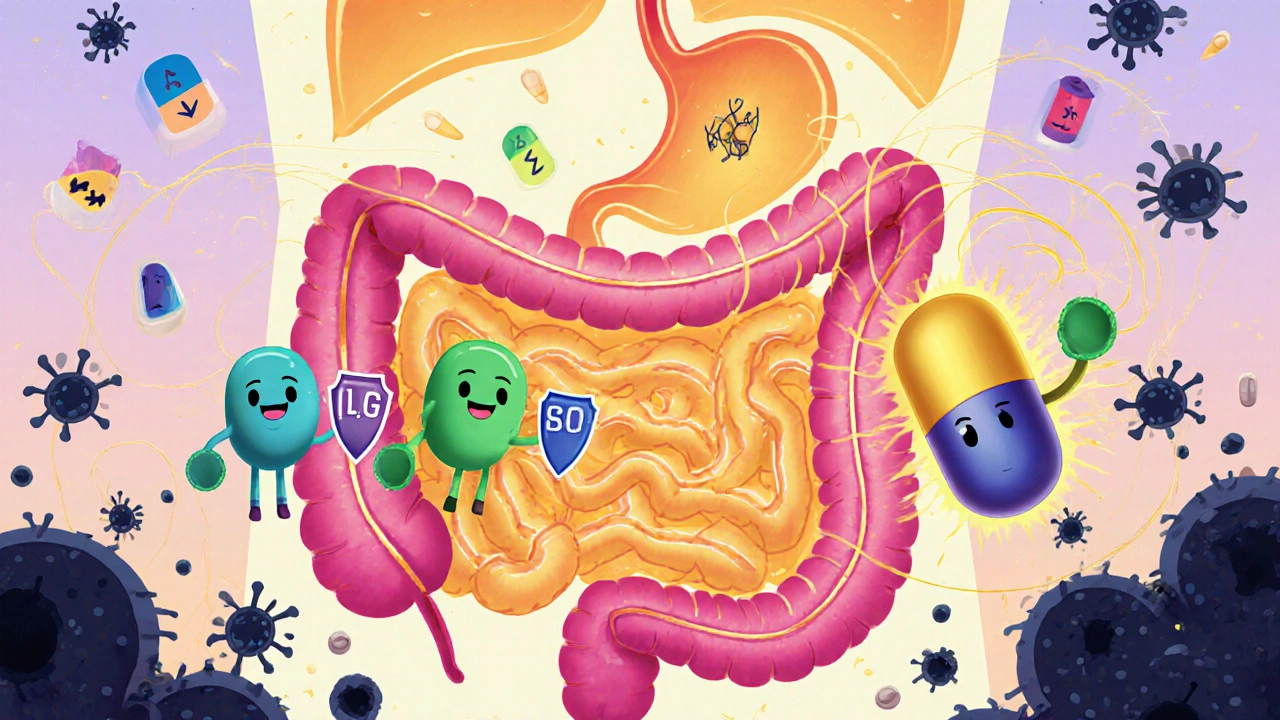
When you take probiotics with antibiotics, live microorganisms that support gut health, often used to counteract antibiotic disruption. Also known as beneficial bacteria, they don't fight infection—they help your body recover from the collateral damage antibiotics cause. Antibiotics wipe out bad bacteria, sure, but they also clear out the good ones that keep your digestion running smoothly. That’s why so many people end up with diarrhea, bloating, or worse after a course of pills. The question isn’t whether probiotics help—it’s which ones, when, and how much.
Not all probiotics are the same. Lactobacillus rhamnosus GG, a well-studied strain shown to reduce antibiotic-associated diarrhea in clinical trials has solid evidence backing it. So does Saccharomyces boulardii, a yeast-based probiotic that survives antibiotics and helps restore gut balance. These aren’t just supplements you pick off the shelf because the label says "supports digestion." They’re targeted tools. Studies show taking them during and right after antibiotics cuts the risk of diarrhea by nearly 50% in adults and kids alike. But if you grab a random blend with 20 strains and no dosing info? You’re gambling.
Timing matters too. Taking probiotics at the same time as your antibiotic? That’s like sending firefighters into a burning house while the arsonist’s still lighting matches. Best practice: space them out by at least two hours. Take the antibiotic, wait, then take the probiotic. And don’t stop too soon—keep going for at least a week after finishing the antibiotics. Your gut needs time to rebuild.
Some people swear by yogurt or kefir instead of pills. Fine, if you’re healthy and eating a lot of it. But a single serving won’t give you the dose you need—most effective probiotic supplements contain billions of live cultures per pill. Yogurt? Maybe a few hundred million. Plus, many commercial yogurts are loaded with sugar, which can feed the wrong kind of bacteria. If you’re fighting antibiotic-related gut chaos, you need precision, not guesswork.
There’s one big exception: if you’re immunocompromised, have a central line, or are in the ICU, probiotics can be risky. In rare cases, the "good" bacteria can cause infections. Always talk to your doctor first if you’re seriously ill or on multiple meds. But for most people—parents, students, office workers, anyone who’s ever had to cancel plans because of antibiotic diarrhea—probiotics are a simple, low-cost way to avoid a miserable side effect.
What you’ll find below are real-world stories and data-backed guides on how people manage this exact issue. From tracking symptoms with a medication journal to choosing the right strain without getting fooled by marketing, these posts cut through the noise. You’ll see how others handled nausea after amoxicillin, what worked for someone on a month-long course of clindamycin, and why some probiotics just don’t play nice with certain antibiotics. No fluff. No hype. Just what helps—and what doesn’t.
Probiotics During Antibiotic Therapy: How to Reduce GI Side Effects
Probiotics can reduce antibiotic-related diarrhea by up to 70% when taken correctly. Learn which strains work, how to time them, and what to avoid for safer gut health during antibiotic treatment.
View More