Overdose Risk: What You Need to Know About Dangerous Drug Interactions
When we talk about overdose risk, the dangerous outcome that happens when the body can’t handle the amount or combination of substances taken. Also known as drug toxicity, it’s not always about taking too much at once—it’s often about how medicines interact in ways you never expected. Many people think overdose only happens with illegal drugs or accidental pill swallowing. But the truth? Most overdose cases in hospitals today come from prescription meds mixed with over-the-counter drugs, supplements, or even foods like grapefruit.
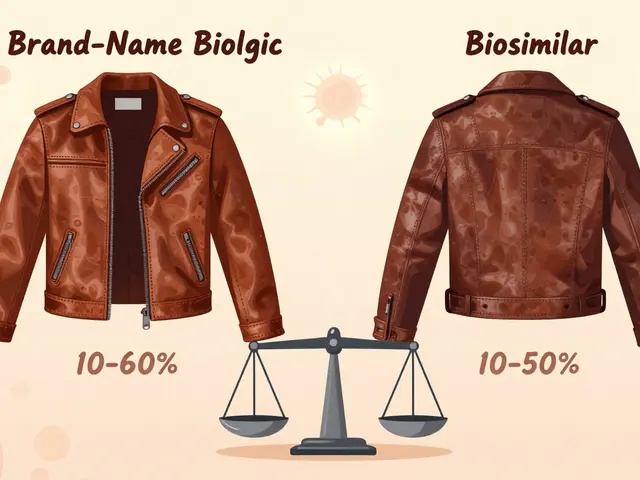
Drug interactions, when two or more substances change how each other works in your body are the silent engine behind many overdose events. Take statins and grapefruit—eating half a grapefruit can turn a safe dose of amlodipine or felodipine into a heart-stopping threat. Or SSRIs like paroxetine, which thin your blood by messing with platelets, making even a minor cut riskier if you’re also on aspirin or ibuprofen. These aren’t rare edge cases. They’re everyday dangers hidden in plain sight. And with generic drug contamination, the presence of harmful chemicals like NDMA or benzene in otherwise approved medications making headlines, you can’t assume safety just because a pill is cheap or labeled "generic."
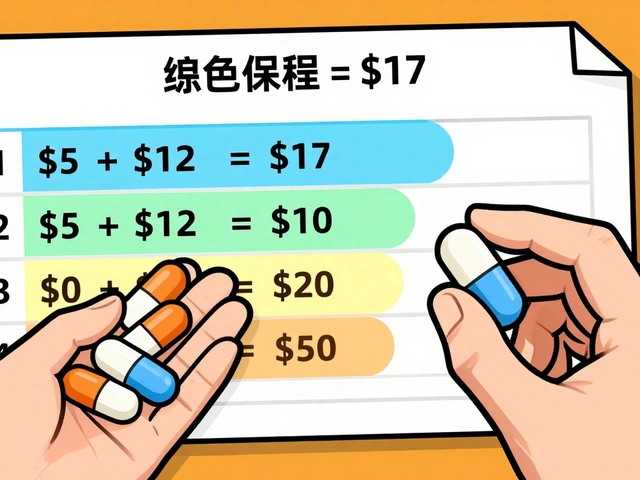
Some meds are especially tricky because of their narrow therapeutic index, the tiny gap between a helpful dose and a toxic one. Levothyroxine, phenytoin, and warfarin fall into this category. Switch brands? Skip a dose? Mix with another drug? That’s when things go sideways fast. Even something as simple as switching from one generic thyroid pill to another can send your TSH levels into chaos if you don’t get checked. And if you’re on multiple meds for heart issues, diabetes, or mental health, you’re playing with fire unless you track every interaction.
Overdose symptoms aren’t always dramatic. They don’t always mean collapsing or vomiting. Sometimes it’s just a weird headache, sudden dizziness, unexplained bruising, or feeling more anxious than usual after starting a new pill. These are warning signs—not just side effects. People ignore them because they think, "It’s just my body adjusting." But adjusting doesn’t mean your liver is shutting down or your blood won’t clot anymore.
What you’ll find below isn’t just a list of articles—it’s a practical toolkit. You’ll see real comparisons between drugs like bupropion and SSRIs, how Prazosin stacks up against alternatives for PTSD, why citrus can turn your blood pressure meds into poison, and how contaminated generics like Mucinex have put people in danger. These aren’t theory pieces. They’re based on real cases, real data, and real people who got hurt because no one told them what to watch for. Whether you’re managing chronic pain, depression, high blood pressure, or just taking a daily vitamin, you need to know what’s hiding in your medicine cabinet—and how to stop it before it stops you.

How to Talk to Your Doctor About Overdose Risk Without Being Judged
Learn how to talk to your doctor about overdose risk using clear, evidence-based language that reduces stigma and increases your chances of getting life-saving help like naloxone.
View More