Arrhythmia Risk: What Medications, Supplements, and Conditions Increase Your Chance of Irregular Heartbeat
When your heart skips, races, or beats unevenly, it’s not just a flutter—it could be arrhythmia risk, the likelihood of developing an abnormal heart rhythm that can lead to stroke, heart failure, or sudden cardiac arrest. Also known as cardiac arrhythmia, this condition doesn’t always cause symptoms, but when it’s triggered by a drug, supplement, or underlying health issue, the consequences can be life-threatening. Many people don’t realize that everyday pills—like certain antibiotics, antidepressants, or even herbal teas—can disrupt the electrical signals in your heart. The risk isn’t just about old age or heart disease; it’s often hidden in what you take daily.
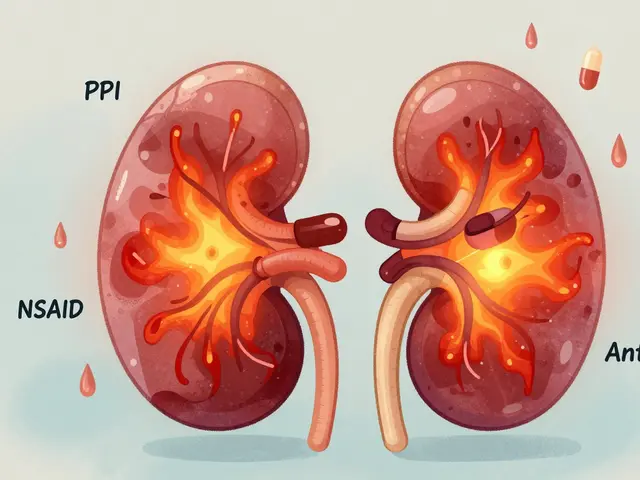
Drug-induced arrhythmia, a type of arrhythmia caused by medications rather than heart damage is more common than you think. Studies show that over 100 prescription and over-the-counter drugs can affect heart rhythm, especially when combined. For example, mixing certain antibiotics like azithromycin with heart meds like amiodarone can spike your risk. Even common painkillers like NSAIDs can worsen arrhythmia in people with existing heart conditions. And it’s not just prescriptions—supplement interactions, how herbal products like St. John’s wort or green tea extract interfere with heart medications—are a silent danger. People think "natural" means safe, but many supplements alter how your body processes drugs, leading to dangerous buildup or sudden drops in medication levels.
Heart medication interactions, when two or more cardiac drugs clash and destabilize rhythm are another major concern. Beta-blockers, calcium channel blockers, and antiarrhythmics are meant to stabilize your heart—but when paired with the wrong other drug, they can do the opposite. Take a common combo: a statin for cholesterol plus a macrolide antibiotic. That mix can raise the risk of torsades de pointes, a dangerous type of arrhythmia. Even something as simple as grapefruit juice can amplify the effect of some heart meds, turning a safe dose into a risky one. And if you’re on multiple meds for high blood pressure, diabetes, or depression, your chances of a hidden interaction go up fast.
What makes this even trickier is that symptoms often show up late—or not at all. You might feel fine until your heart suddenly starts pounding, or you get dizzy standing up. That’s why tracking what you take matters. If you’re on more than three medications, keeping a simple list—including supplements and OTC drugs—can help your doctor spot red flags before they become emergencies. The posts below break down exactly which drugs carry the highest arrhythmia risk, how to read labels for hidden dangers, and what to do if you’re on a medication that might be affecting your heartbeat. You’ll find real-world examples of how people avoided cardiac side effects by catching problems early, and which supplements are safest (and which aren’t) when you have a history of irregular rhythm. No guesswork. Just clear, practical steps to protect your heart.

Macrolides and QT-Prolonging Drugs: Understanding the Arrhythmia Risk
Macrolide antibiotics like azithromycin and clarithromycin can prolong the QT interval, increasing the risk of life-threatening arrhythmias. Learn who's most at risk, how to spot danger signs, and safer alternatives.
View More