Antifungal Treatment: How to Choose the Right Therapy
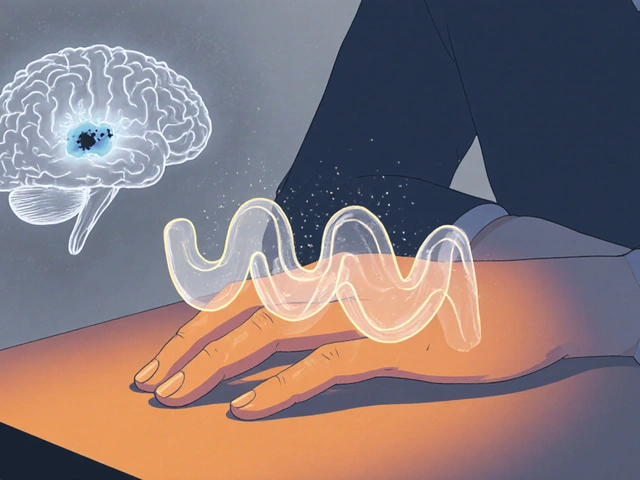
When dealing with antifungal treatment, the use of medicines to eliminate or control fungal infections in humans or animals. Also known as antifungal therapy, it is essential for stopping the spread of harmful fungi. A fungal infection, any condition caused by the growth of fungi on skin, nails, or internal organs can range from a mild athlete’s foot to a life‑threatening systemic disease. Understanding that antifungal treatment encompasses both topical antifungal, creams, sprays, or powders applied directly to the affected area and systemic antifungal, oral tablets or intravenous drugs that travel through the bloodstream is the first step toward an effective plan. Accurate diagnosis influences every decision, because the type of fungus, its location, and the patient’s health status dictate whether a cream will suffice or an oral prescription is required. This relationship forms a core semantic triple: accurate diagnosis → informs antifungal treatment choice → improves outcomes.
Key Considerations for Effective Antifungal Treatment
Choosing the right medication means weighing several factors. First, the severity of the infection decides if a topical antifungal like clotrimazole or terbinafine cream will work; mild skin infections often clear up with a few weeks of consistent use. For deeper or widespread infections, a systemic antifungal such as fluconazole, itraconazole, or amphotericin B becomes necessary to reach the fungus wherever it hides. Second, patient-specific issues—liver function, kidney health, drug interactions—shape the safety profile of the chosen drug. Third, the growing problem of drug resistance, when fungi mutate and become less responsive to standard therapies forces clinicians to consider newer agents or combination therapy. In practice, this creates another semantic triple: rising drug resistance → prompts alternative or combo therapy → ensures successful antifungal treatment.
Beyond the clinical side, practical steps help patients get the most out of their therapy. Always follow the prescribed duration, even if symptoms fade early; stopping too soon can let the fungus rebound. Keep the affected area clean and dry, especially for skin infections, because moisture fuels fungal growth. When using oral agents, take them with food if recommended, and monitor any side effects like nausea or liver discomfort. If you notice no improvement after the expected time, contact a healthcare professional—persistent infection may signal resistance or a misdiagnosis. By understanding how antifungal treatment ties together diagnosis, medication type, and resistance patterns, you’re better equipped to manage fungal infections safely and effectively. Below, you’ll find a curated list of articles that dive deeper into specific drugs, comparison guides, and tips for buying safe generics online.
How Voriconazole Treats Fungal Peritonitis: Dosage, Effectiveness, and Key Considerations
Voriconazole is a key antifungal for treating fungal peritonitis, especially in dialysis patients. Learn how it works, when to use it, and what to watch for to avoid treatment failure.
View More
5 Common Myths About Fungal Skin Discoloration - Debunked
Debunk the top five myths about fungal skin discoloration, learn the real causes, effective treatments, and how to prevent recurrences.
View More