
What Are NTI Drugs and Why Do They Matter?
Narrow Therapeutic Index (NTI) is a term used for medications where the difference between a safe, effective dose and a harmful or ineffective dose is extremely small. These drugs don’t allow much room for error. A tiny change in blood levels-just a few percentage points-can mean the difference between controlling a seizure, preventing organ rejection, or triggering toxicity.
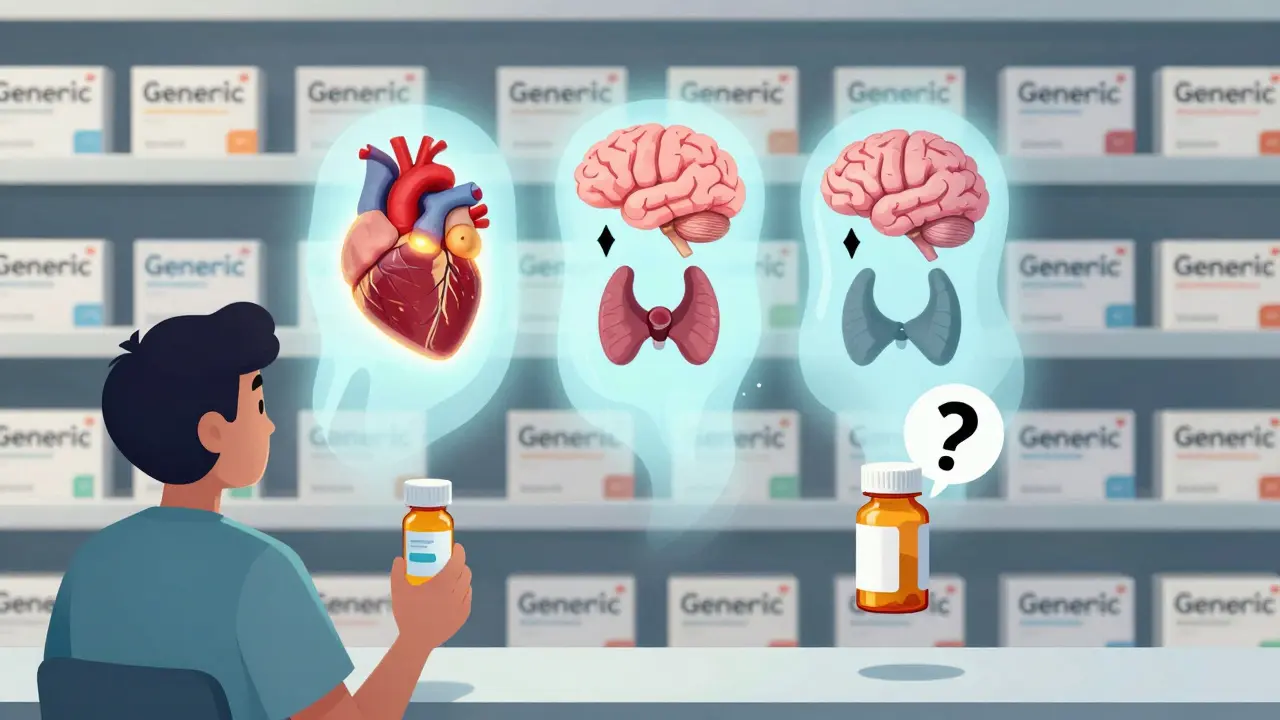
Common NTI drugs include warfarin (used to prevent blood clots), levothyroxine (for thyroid replacement), digoxin (for heart rhythm), lithium (for bipolar disorder), and carbamazepine and phenytoin (for epilepsy). Even small shifts in how these drugs are absorbed or metabolized can lead to serious outcomes: a stroke, a seizure, kidney damage, or even death.
Why Switching Between Generic Manufacturers Can Be Risky
The FDA approves generic drugs as therapeutically equivalent to brand-name versions. That’s the official line. But for NTI drugs, the reality on the ground is more complicated. While generics must meet strict bioequivalence standards-95% to 105% of the active ingredient compared to the brand-these limits are tighter than for regular medications (which are allowed 90%-110%). Still, even within that narrow range, differences in inactive ingredients, tablet coatings, or manufacturing processes can affect how quickly or completely the drug enters the bloodstream.
Take tacrolimus, a critical drug for transplant patients. One study found that different generic versions varied in active ingredient content by as much as 14%: one batch had 93%, another had 110%. While the average difference wasn’t statistically significant, individual patients saw wide swings in blood levels. In kidney transplant patients, switching between generic brands of tacrolimus was linked to a 21.9% coefficient of variation in drug concentration-far higher than what’s considered safe.
For levothyroxine, the FDA’s own real-world data shows that 98.7% of patients maintained stable thyroid levels after switching from brand to generic. That sounds reassuring. But a 2015 study in US Pharmacist found that some patients, even with normal lab results, reported fatigue, weight gain, or brain fog after switching manufacturers. These symptoms didn’t show up in blood tests, but they mattered to the people living with them.
What the Data Really Shows About Generic Switching
Let’s be clear: population-level studies often show no major difference in outcomes when switching between generic NTI drugs. A 2019 study on warfarin found that switching between generic manufacturers led to a small but statistically significant increase in INR variability-about 0.32 points higher. That’s not huge, and it didn’t result in more bleeding events over six months. But for a patient on warfarin, even a 0.3 change in INR can push them out of the therapeutic window (2-3), increasing clotting or bleeding risk.
Another study on cyclosporine in transplant patients showed a 15.3% higher rate of acute organ rejection when patients switched from one generic formulation to another. That’s not a statistical anomaly-it’s a clinical red flag. These aren’t theoretical concerns. They’re happening in real patients.
And here’s the catch: pharmacists and doctors don’t always know which generic version a patient is taking. Many states allow automatic substitution, and pharmacy systems often default to the cheapest option. So a patient might be on one generic in January, another in March, and a third in June-all labeled the same, all approved by the FDA, but potentially delivering different results.
Why Do Some Doctors and Patients Still Worry?
Despite FDA assurances, many clinicians remain cautious. The American Academy of Neurology, for example, recommends against automatic substitution of generic antiepileptic drugs. Why? Because seizures don’t care about bioequivalence studies. They care about consistent blood levels. A patient who’s been stable on one generic for years might suddenly have breakthrough seizures after a pharmacy switch-not because the drug is bad, but because their body reacted to a subtle change in how it absorbed the medication.
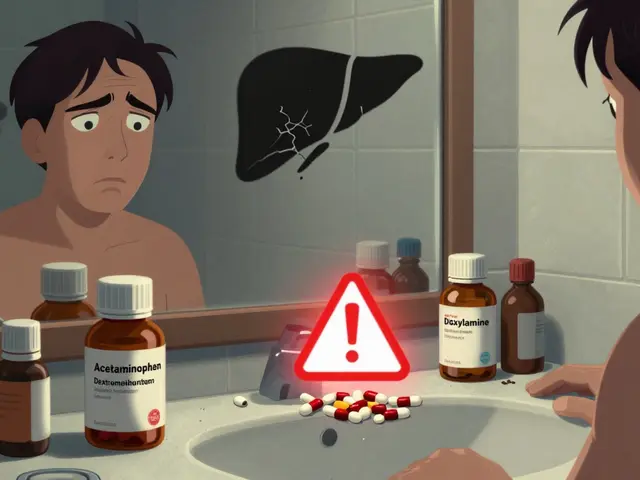
Patients with chronic conditions are especially vulnerable. Someone on lithium for bipolar disorder needs levels kept between 0.6 and 1.0 mEq/L. Go above 1.2, and you risk tremors, confusion, or kidney damage. Go below 0.5, and depression or mania can return. If a new generic batch delivers even 5% less lithium, the patient might not feel the difference until they’re in crisis.
Pharmacists report that 63% have received complaints from patients or doctors after switching NTI generics. These aren’t just anecdotes. They’re patterns. One patient might tolerate three different generics without issue. Another might react to the first switch. There’s no way to predict who will be affected.
How States Are Handling the Issue
As of 2022, 27 U.S. states have laws that restrict or require special consent before substituting NTI drugs. In these states, pharmacists must notify the prescriber or get explicit permission before switching a patient from one generic to another. Some states require the prescription to be labeled “Do Not Substitute” for NTI drugs like phenytoin or valproic acid.
But in the other 23 states, substitution is automatic. Patients often don’t know they’ve been switched. And if they do notice something’s off-feeling tired, dizzy, or anxious-they may blame themselves, their diet, or stress, not the medication.
It’s not just about law. It’s about culture. In states with stricter rules, pharmacists are more likely to discuss the risks with patients. In states without, the default is convenience and cost. And for many patients, that’s the only thing that matters.

What You Can Do If You’re Taking an NTI Drug
- Ask your doctor to write “Dispense as Written” or “Do Not Substitute” on your prescription. This legally prevents the pharmacy from switching brands without your doctor’s approval.
- Check the name on your pill bottle. Generic drugs often list the manufacturer (e.g., “Levothyroxine by Teva” or “Warfarin by Mylan”). Keep track of which one you’re on. If it changes, call your doctor.
- Get regular blood tests. If you’re on warfarin, digoxin, lithium, or tacrolimus, make sure your levels are checked consistently-especially after any switch.
- Report any changes in how you feel. Even small symptoms like increased anxiety, tremors, or unexplained fatigue could signal a problem. Don’t dismiss them.
- Ask your pharmacist: “Is this the same manufacturer as last time?” If they don’t know, it’s a sign you need to be more involved.
The Bigger Picture: Why This Isn’t Just About Generics
Here’s something most people don’t realize: brand-name manufacturers change their formulations too. A drug made by Pfizer today might be different from the one made last year. The FDA doesn’t require retesting every time a brand changes its filler or coating. So if you’re worried about generic switching, you should also be aware that brand-name versions aren’t always the same either.
The real issue isn’t generics versus brands. It’s consistency. For NTI drugs, the same manufacturer, same formulation, same batch-over time-is the safest approach. That’s why some patients do better on one generic than another. It’s not that one is better. It’s that their body adapted to one specific version.
Until we have a system that tracks every pill’s manufacturer and formulation at the point of dispensing, patients will continue to be caught in the middle. The FDA says these drugs are interchangeable. But for the people taking them, the question isn’t about science-it’s about safety, stability, and trust.
Final Thoughts
NTI drugs are not like your everyday painkiller or antibiotic. They demand precision. And while the FDA’s approval process is rigorous, it’s designed for populations-not individuals. What works for 98 out of 100 patients might not work for the one who’s sensitive to a slight change in absorption. That’s why awareness, communication, and vigilance matter more than ever.
If you’re on an NTI drug, don’t assume that “generic” means “identical.” Stay informed. Ask questions. Track your levels. And don’t let cost savings come at the price of your health.
Are all generic NTI drugs the same?
No. While all FDA-approved generics must meet bioequivalence standards, they can differ in inactive ingredients, tablet coatings, and manufacturing processes. These small differences can affect how quickly or completely the drug is absorbed, especially in NTI drugs where even minor changes can impact safety or effectiveness.
Can I switch between generic brands of levothyroxine safely?
Many patients switch without issue, and FDA data shows most maintain stable TSH levels. However, some individuals report symptoms like fatigue or weight changes after switching. Because thyroid levels are so sensitive, it’s best to stick with the same manufacturer unless your doctor approves a change and monitors your TSH closely afterward.
Why do some doctors refuse to allow generic substitution for NTI drugs?
Some doctors, especially neurologists and transplant specialists, have seen patients experience adverse events after switching generics-like breakthrough seizures or organ rejection. Even though population studies show no major risk, individual variability is real. These doctors prioritize consistency over cost savings.
How do I know which generic manufacturer I’m getting?
Check the label on your pill bottle. Generic manufacturers are usually listed (e.g., Teva, Mylan, Accord). If it’s not clear, ask your pharmacist. You can also ask your doctor to write “Dispense as Written” on your prescription to prevent automatic switching.
Should I avoid generics altogether if I’m on an NTI drug?
Not necessarily. Many people take generic NTI drugs safely for years. The key is consistency. If you start on a generic, try to stay on the same manufacturer. Don’t switch unless your doctor recommends it-and always monitor your blood levels after any change.
2 Comments
vivian papadatu
February 2 2026
This is one of those issues where policy fails the individual. The FDA’s population-level data is statistically sound, but medicine isn’t a spreadsheet. People aren’t averages. I’ve seen patients with perfect TSH levels still feel awful after a switch - fatigue, brain fog, mood swings. Those aren’t 'in their head.' They’re real. Consistency isn’t luxury - it’s clinical necessity for NTI drugs.




Aditya Gupta
February 1 2026
Bro, just stick with one generic. I switched my levothyroxine and felt like a zombie for two weeks. Turns out the new batch had different fillers. My doctor didn't even know I'd been switched. Don't let the pharmacy play roulette with your hormones.