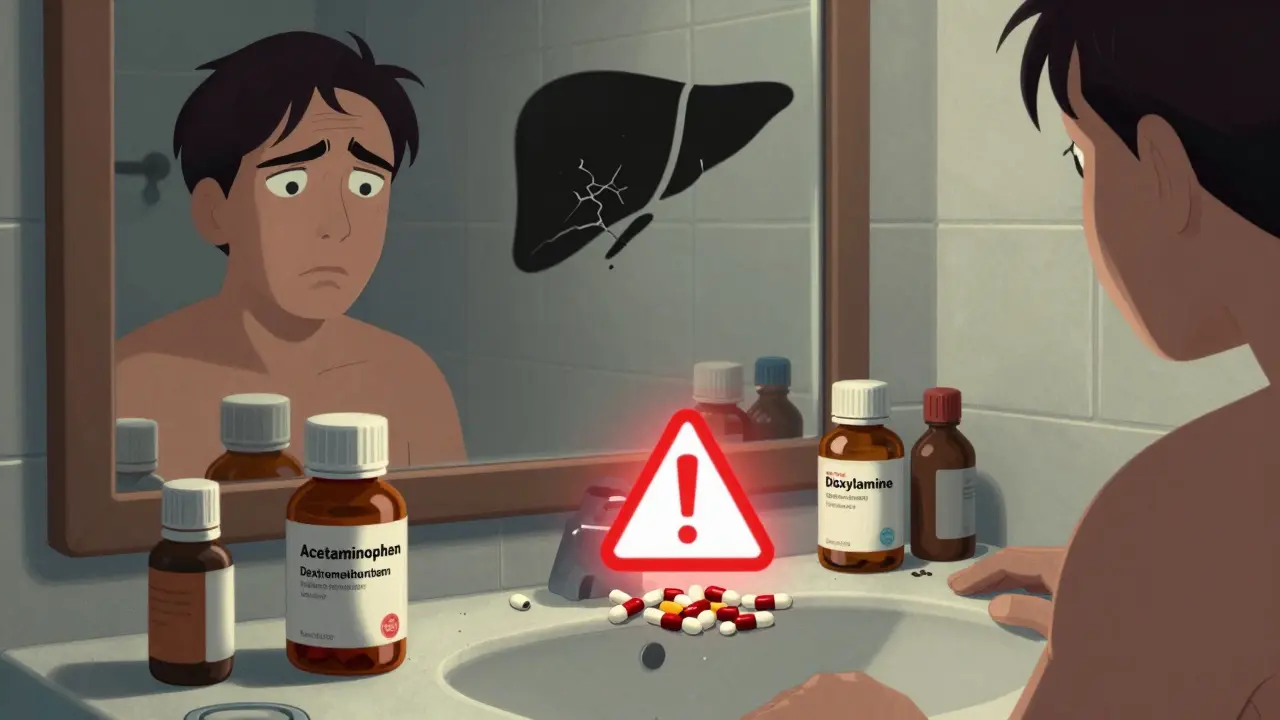
Every winter, millions of people reach for OTC cold and flu combinations thinking they’re making things easier. One pill for fever, one for cough, one for congestion - all in a single box. Sounds smart, right? But here’s the truth: acetaminophen is hiding in more than 70% of these products. And if you’re taking more than one, you could be poisoning your liver without even knowing it.
What’s Actually in Those Combination Pills?
OTC cold and flu medicines aren’t magic. They’re mixtures of active ingredients, each targeting a different symptom. The most common ones you’ll find:- Acetaminophen (also called paracetamol or APAP) - for fever and pain
- Dextromethorphan (often labeled as DM) - to suppress cough
- Phenylephrine - a nasal decongestant (though it’s increasingly proven to not work at OTC doses)
- Doxylamine or chlorpheniramine - antihistamines that cause drowsiness, used in nighttime formulas
- Ibuprofen - an alternative to acetaminophen in some products like Advil Cold & Flu
Why Double Dosing Happens (And Why You’re Not Alone)
You’re not careless if you’ve accidentally doubled up. You’re just human. Here’s how it usually goes:- You take DayQuil for your stuffy nose and cough in the morning.
- By afternoon, your head still hurts, so you grab a Tylenol from the cabinet.
- At night, you take NyQuil because you can’t sleep.
The Hidden Dangers Beyond Acetaminophen
Acetaminophen is the biggest risk, but it’s not the only one. Take doxylamine, the sleep-inducing antihistamine in NyQuil. It can last 8-12 hours. If you take it at 10 p.m. and have to wake up early for work, you might feel groggy, dizzy, or even impaired - like you had a drink. That’s not normal tiredness. That’s a drug effect. And if you take it again the next night, the buildup can make you feel worse than the cold itself. Phenylephrine, the decongestant in most daytime formulas, has been under fire for years. Studies show it doesn’t work at the 10mg dose used in OTC products. The FDA proposed removing it from the approved list in late 2024. Yet, it’s still in nearly every shelf product. You’re paying for something that doesn’t work - and getting extra chemicals you don’t need. And then there’s pseudoephedrine, the real decongestant found in Sudafed. It’s kept behind the pharmacy counter because it can be used to make meth. But if you’re looking for a decongestant and grab phenylephrine instead, you’re wasting your time - and your money.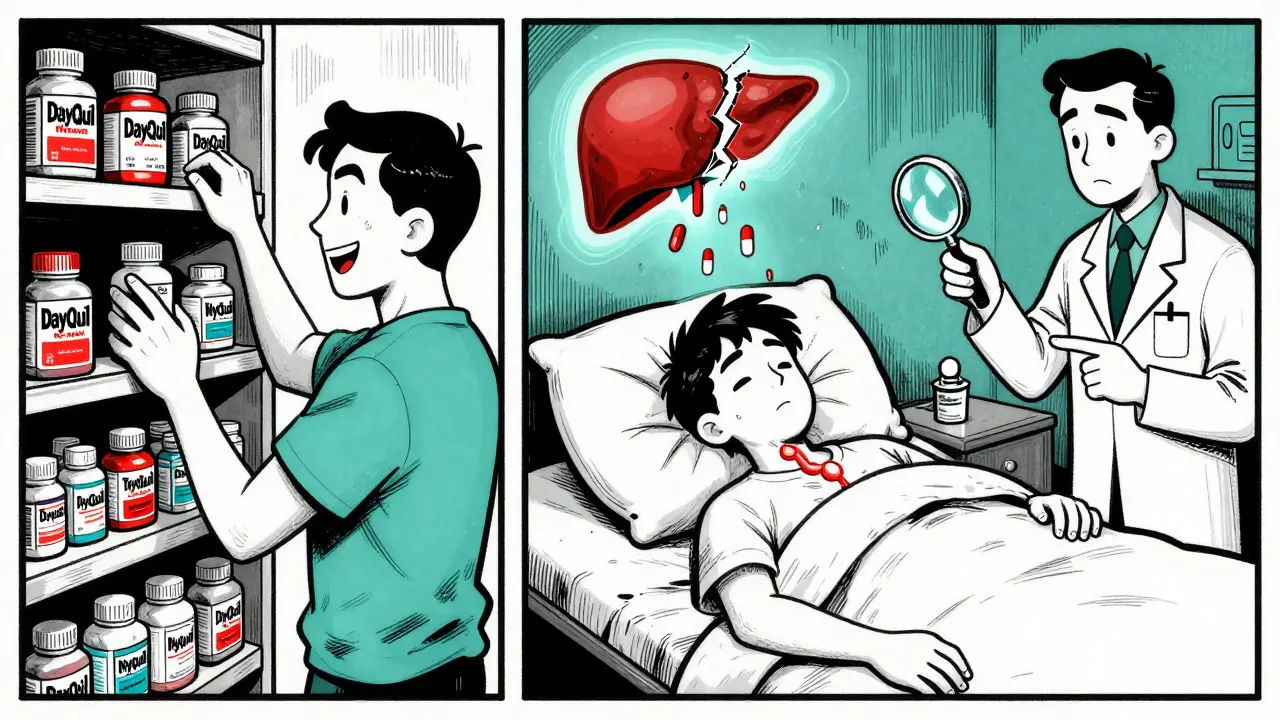
What Experts Actually Recommend
Pharmacists don’t recommend combination products. Not because they’re dangerous - they’re not, if used correctly - but because they’re usually unnecessary. A 2022 survey of 1,200 pharmacists found that 68% prefer to recommend single-ingredient medicines. Why? Because you only take what you need. If you have a fever and a sore throat, take acetaminophen. If you have a cough, take dextromethorphan. If you’re congested, try a saline spray or a decongestant nasal spray - not a pill with five ingredients you don’t need. Dr. Sarah Ketchen, a family physician and spokesperson for the American Academy of Family Physicians, says: “About 65% of patients don’t realize acetaminophen is in multiple cold medications. They think they’re helping themselves - but they’re risking liver damage.” And it’s not just liver damage. Mixing antihistamines with alcohol? Dangerous. Taking decongestants if you have high blood pressure? Risky. Using these pills long-term? Not safe. These aren’t vitamins. They’re drugs. And drugs have side effects.How to Use OTC Cold Medicine Without Risking Your Health
Here’s what you actually need to do - no fluff, no guesswork.- Read the Drug Facts label - every time. Don’t just look at the brand name. Open the box. Flip it over. Find the “Active Ingredients” section. That’s where the truth is. Write down the name and dose of each ingredient.
- Know your ingredients. Acetaminophen = APAP = paracetamol. Dextromethorphan = DM. Phenylephrine = decongestant. Doxylamine = nighttime sleep aid. If you see any of these on two different bottles, don’t take both.
- Use a medication tracker. Keep a notepad or use your phone. Write down what you took, when, and how much. Even if you think you won’t forget - you will.
- Don’t mix with alcohol. It increases liver damage risk and makes drowsiness worse.
- Check other meds too. Many prescription painkillers, sleep aids, and even some antidepressants contain acetaminophen. Your pharmacist can help you check this.
- Ask your pharmacist. They’re trained for this. Take your bottle in. Say, “I’m taking this for a cold. Is it safe with what else I’m on?” It takes five minutes. It could save your liver.
When to Skip Combination Products Altogether
You don’t need them if:- You only have one or two symptoms (e.g., just a cough or just a headache)
- You’re over 65 - your body processes drugs slower
- You have liver disease, high blood pressure, or are pregnant
- You’re taking other medications - even herbal ones like St. John’s Wort
- You’ve had a reaction to any cold medicine before

What’s Changing in the Cold Medicine Market
The industry is shifting. In November 2024, the FDA proposed removing oral phenylephrine from OTC products because it doesn’t work. That means next winter, you’ll see fewer products with it. Manufacturers are already testing alternatives - like guaifenesin, which helps loosen mucus, not just stuff your nose. Sales data shows a quiet revolution: single-ingredient acetaminophen sales rose 12.7% in 2023. Combination cold medicine sales? Only 2.3%. People are starting to wake up. And the next wave? Products that combine fewer ingredients - maybe three instead of four or five. Or even smart packaging: one tablet for daytime, one for nighttime, clearly labeled so you can’t mix them up.What to Do If You Think You’ve Overdosed
If you’ve taken more than the recommended dose of acetaminophen - even if you feel fine - call Poison Control immediately: 1-800-222-1222. Liver damage from acetaminophen doesn’t always show symptoms right away. You might feel fine for 24 hours - then suddenly get nauseous, pale, and confused. By then, it’s too late. Don’t wait. Don’t Google it. Call. It’s free. It’s confidential. And it saves lives.Can I take Tylenol and DayQuil together?
No. Both contain acetaminophen. Taking them together can easily push you over the 4,000mg daily limit, which can cause serious liver damage. If you need extra pain relief, skip the Tylenol and use a non-acetaminophen option like ibuprofen - but only if you don’t have stomach or kidney issues.
Is phenylephrine still in cold medicines?
Yes, for now. But the FDA proposed removing it in late 2024 because studies show it doesn’t work at the 10mg dose used in OTC products. Manufacturers have until 2026 to reformulate. Look for products labeled “phenylephrine-free” or switch to pseudoephedrine (behind the counter) if you need a real decongestant.
Why do nighttime cold medicines make me so groggy the next day?
Because they contain antihistamines like doxylamine or diphenhydramine, which aren’t just sleep aids - they’re long-acting sedatives. They can linger in your system for over 12 hours. That’s why you feel foggy, slow, or unsteady the next morning. If you need to drive or work, avoid nighttime formulas.
Are store-brand cold medicines the same as name brands?
Yes, almost always. CVS Health, Walgreens, and Equate versions use the same active ingredients and doses as Tylenol, Vicks, or Theraflu. The only differences are the inactive fillers and packaging. Save your money - read the Drug Facts label. If the active ingredients match, it’s the same medicine.
What’s the safest way to treat a cold without pills?
Rest, fluids, and time. Use saline nasal sprays for congestion, honey for cough (if over age 1), and warm broth for sore throat. For fever or pain, a single dose of acetaminophen or ibuprofen is fine - just don’t combine it with other meds. Most colds clear up in 7-10 days. Pills don’t cure them - they just make them more bearable.






Candice Hartley
January 27 2026
Just took NyQuil last night and woke up feeling like a zombie. Not tired. ZOMBIE. 🤯