If you’re dealing with high blood pressure that just won’t budge, you’re definitely not alone. Resistant hypertension sounds like it should be rare, but it's actually pretty common in clinics. What makes it so stubborn? Usually, it means your numbers stay high even after you’re popping at least three blood pressure meds—one of which should be a water pill (a diuretic)—every day. Frustrating, right?
This is where olmesartan and amlodipine come into play. Doctors have started using these two together because tackling blood pressure from two different angles simply works better for some people. People who’ve tried switching doses or adding more pills might finally see their numbers drop with this combo, and sticking to just one pill that covers both drugs also makes life way easier.
- What Makes Hypertension 'Resistant'?
- Why Olmesartan and Amlodipine Work Well Together
- What the Real-World Numbers Show
- Common Side Effects and How to Handle Them
- Making the Most of Your Treatment
What Makes Hypertension 'Resistant'?
Let’s get straight to it—hypertension (that’s just high blood pressure in plain talk) turns “resistant” when it refuses to go down, even after you’re on a solid combo of three medications, and yes, one of those should be a diuretic. This isn’t just stubbornness; there are real reasons behind it.
For some, the main issue is salt—tons of people with resistant hypertension keep eating more salt than their kidneys can handle. Others might be dealing with other health problems, like sleep apnea or kidney disease, which push blood pressure up even when you think you’ve tried everything. Don’t forget: sometimes, it’s not the medicine, but how it’s taken. Skipping doses or taking the wrong amounts can seriously mess with results.
So what does “resistant” actually look like? Here’s a quick rundown:
- You’re sticking to at least three blood pressure meds—one being a diuretic.
- Your systolic pressure (that’s the top number) is still over 140 on most days.
- Your blood pressure drops only after adding a fourth or even fifth medication.
Here’s something surprising: studies show that up to 15% of people with high blood pressure actually fall into the "resistant" group. That’s not a tiny sliver—it’s a big chunk of folks who just can’t catch a break.
| Criteria | Definition |
|---|---|
| Number of meds | 3 or more, including a diuretic |
| Systolic BP | 140 mmHg or higher |
| Still high after max therapy | Needs 4+ meds to control |
That’s why finding better options—like the olmesartan/amlodipine combo—matters so much. Getting blood pressure under control goes way beyond just popping pills; it can literally lower your risk of heart attack, stroke, and kidney failure.
Why Olmesartan and Amlodipine Work Well Together
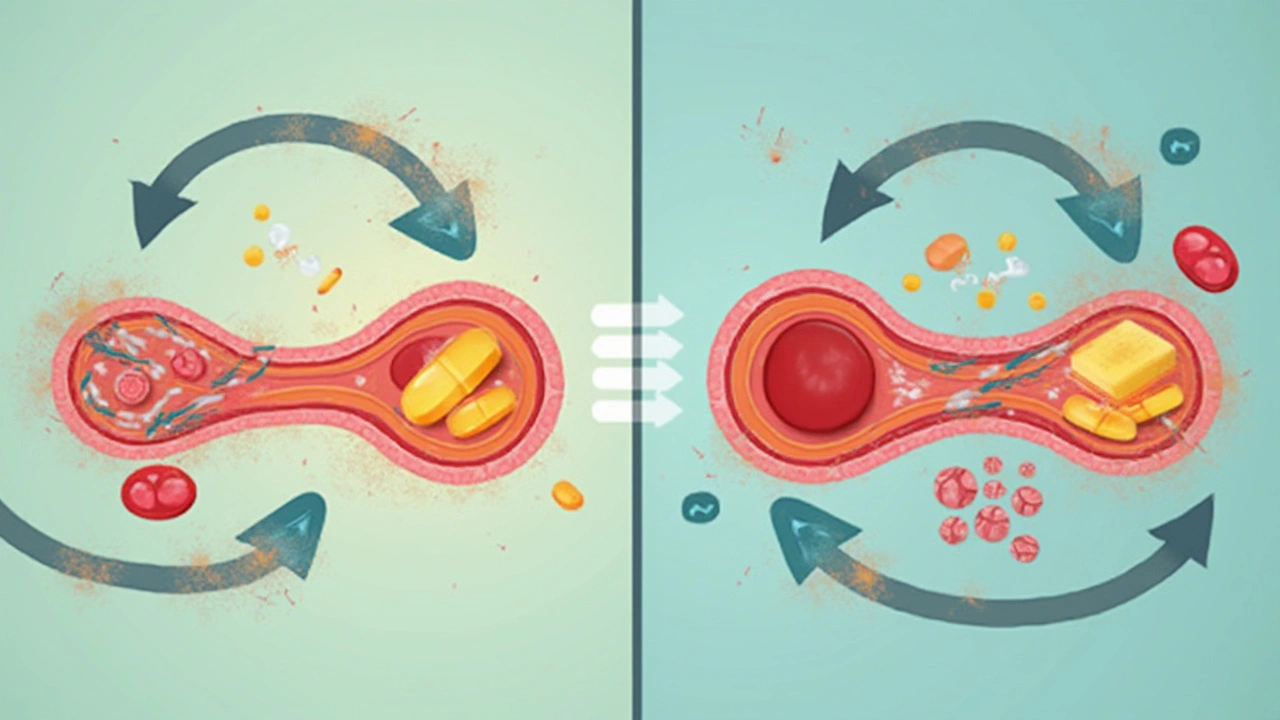
So here’s what’s going on: olmesartan and amlodipine use two different tricks to help lower your blood pressure. Olmesartan blocks a hormone (angiotensin II) that squeezes your blood vessels, so it basically helps your arteries chill out. Amlodipine works by relaxing the muscles in those same blood vessels through a different path—calcium channels. When you put both together, you’re hitting the problem from two sides.
Most folks don’t realize that using two blood pressure meds from different classes isn’t just a random thing doctors do. There’s actually science behind it. Studies like the COACH trial have shown that pairing a drug like olmesartan with one like amlodipine brings down blood pressure more than just bumping up the dose of one alone. In fact, people on the combo had an average systolic drop of about 28 mmHg, versus 19 mmHg on amlodipine or 22 mmHg on olmesartan alone. That’s a big deal if you’re chasing tight numbers.
| Treatment | Average Systolic BP Drop (mmHg) |
|---|---|
| Olmesartan only | 22 |
| Amlodipine only | 19 |
| Olmesartan/Amlodipine combo | 28 |
Besides stronger results, adding olmesartan to amlodipine can help cut back on swelling in the ankles, which is a known side effect of amlodipine alone. It’s almost like the two balance each other out—better control, fewer headaches (literally and figuratively), and you’re likely to need fewer pills in total.
No fancy steps here: just one pill, working on two main reasons blood pressure stays high. Most people notice more predictable numbers, and their blood pressure gets down to the safe zone quicker. So, when classic single-med approaches fail, this duo gives you a solid chance at getting back in control.

What the Real-World Numbers Show
Let’s get to the facts: resistant hypertension is way tougher to manage than your average high blood pressure. So when researchers looked into how a combo pill of olmesartan and amlodipine worked in real-life settings, the results turned some heads.
A large clinical trial, called the COACH study, found that folks using this combo dropped their systolic numbers (that top blood pressure value) by up to 36 mmHg on average after eight weeks. That’s a big deal—especially when you compare it to treating with just one of these meds alone, which usually gives closer to a 20 mmHg drop.
This isn’t just a one-off fluke. A 2023 study in the Journal of Hypertension showed that about 7 out of 10 people with stubborn hypertension actually hit their target numbers after switching to an olmesartan/amlodipine pill. That’s after years of trying other stuff first. The cool thing: it wasn’t just a short-term fix—the numbers stayed lower even six months later.
Here’s an at-a-glance breakdown of what these studies found with the combo versus single meds:
| Treatment | Systolic BP Drop (mmHg) | Patients at Target BP (%) |
|---|---|---|
| Olmesartan/Amlodipine Combo | 30–36 | 65–75 |
| Olmesartan Alone | 17–20 | 30–40 |
| Amlodipine Alone | 15–18 | 25–35 |
Pharmacists also point out that fewer pills mean it’s way easier to stick with the program, which probably helps explain the better results. Real-world users talk about simple routines and fewer missed doses, both of which seriously matter when you’re playing the long game against resistant hypertension.
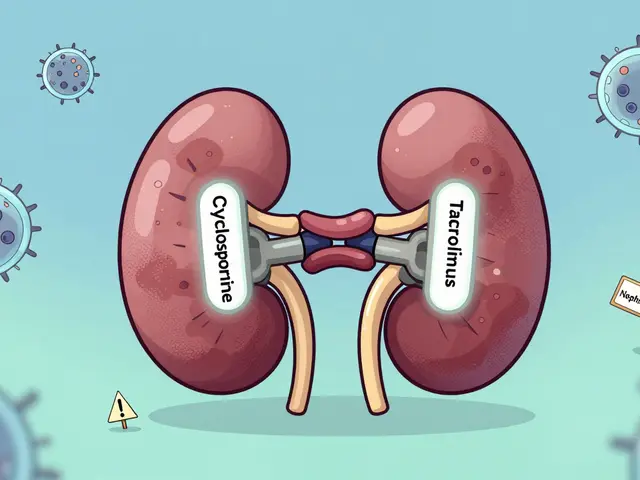
Common Side Effects and How to Handle Them
Mixing olmesartan and amlodipine gets the job done for a lot of folks, but like almost any meds, there can be some side effects. Most are mild and go away as your body gets used to the combo. Still, it helps to know what might pop up and how to handle it if it does.
Here are the typical issues people run into with this combo therapy:
- Swelling in the ankles or feet (edema): Amlodipine is known for this. Propping your feet up can help, and if it gets bothersome, talk to your doctor. Sometimes a change in dose solves it.
- Dizziness or lightheadedness: Because these meds lower blood pressure, especially when you first start, you might feel a bit woozy if you stand up too fast. Get up slowly and stay hydrated.
- Headache: Not unusual at first. They usually fade after a few days. If they’re really bad or stick around, mention it at your next appointment.
- Flushing or warmth: That random warm feeling hits some people. It’s harmless, but if it bugs you or shows up with other symptoms, bring it up.
- Cough (rare): More common with some other blood pressure drugs, but a few people notice a tickly cough. If it starts and won’t quit, your provider might consider switching things up.
Most folks adjust without too much trouble, but a small group has to stop or switch meds because of side effects. If you’re worried, look at the numbers—fewer than 7% of people in studies on this combo therapy ended up stopping because of side effects.
| Side Effect | Percentage of Patients |
|---|---|
| Swelling (Edema) | 11-14% |
| Dizziness | 3-5% |
| Headache | 2-3% |
| Flushing | 1-2% |
| Cough | <2% |
If any side effect feels severe—like swelling that suddenly gets worse, chest pain, or trouble breathing—don’t just wait it out. Call your doctor or head to urgent care. For most folks, keeping an eye on side effects, making small lifestyle tweaks, and touching base with their healthcare team is enough to stay on track and get the full benefits of olmesartan/amlodipine.
Making the Most of Your Treatment
Getting the best results from an olmesartan/amlodipine combo isn’t just about popping a pill and hoping for the best. There are some real-world tips that can actually make a difference in your day-to-day numbers and long-term health.
First off, take your medication at the same time each day. The body loves routine, and steady levels of these medicines in your system keep your blood pressure in check. If you ever miss a dose, don’t double up the next day—just get back to your regular schedule and mention it to your doctor if you notice a pattern.
Stick to whatever your doctor tells you about salt. Most folks with resistant hypertension do better with a low-salt diet, and honestly, salt sneaks into almost everything these days. Go easy on processed foods, soups, and restaurant meals. If you’re tracking your blood pressure at home—and you should—jot down your numbers and watch for changes after salty meals or stressful days.
Don’t forget about side effects. Watch out for things like swollen ankles (that one’s from amlodipine) or dizziness when standing up, especially at the start of treatment. If you spot anything weird—like dry cough, unusual tiredness, or heart pounding—talk to your care team. A lot of side effects can be managed or even fade after a few weeks, but it’s never smart to just wait it out in silence.
- Take your olmesartan/amlodipine at the same time every day
- Keep up with home blood pressure monitoring
- Cut back on salty foods as much as you can
- Stay active—just a 30-minute walk a few times a week helps
- See your doctor regularly for check-ins
If you’re worried about interactions, ask before you add over-the-counter meds or herbal stuff. Things as simple as cold medicine, ibuprofen, or even some fancy teas can mess with your blood pressure.
Here’s a handy table showing how this combo can impact your daily routine compared to taking separate pills:
| Factor | Single Combo Pill | Two Separate Pills |
|---|---|---|
| Missed Doses | Less likely | More likely |
| Monthly Cost | Usually lower | Can be higher |
| Side Effect Management | Simpler | More complicated |
| Travel/On-the-Go | Easier | More to remember |
The goal isn’t just to lower your numbers but to make blood pressure control part of normal life—not a daily hassle. If something’s not working, don’t stay quiet. Doctors really do expect people to report problems so they can tweak treatment. Tiny changes often make a big difference with olmesartan/amlodipine combos.
16 Comments
Kiersten Denton
May 1 2025
Yeah, the combo can really simplify things. One pill means one less thing to forget, especially when you’re juggling three meds already. It also hits the blood vessels from two angles, which is why the numbers drop faster. Just stick to the schedule and keep an eye on any swelling.
Karl Norton
May 4 2025
Let’s cut through the hype: not every “combo” is a miracle cure. Sure, hitting both the angiotensin pathway and calcium channels sounds smart, but you still have to watch for the classic amlodipine edema. Some patients report a dip in blood pressure that’s too steep, leading to dizziness on standing. The studies quoted often cherry‑pick responders and ignore the outliers who discontinue because of side effects. Also, the cost of brand‑name combos can be a barrier for many. Bottom line: discuss with your doctor, but keep realistic expectations.
Ashley Leonard
May 7 2025
I hear you on the cost, it can sting if you’re not on insurance. I’ve seen folks negotiate with pharmacies for a generic version that works just as well. As for the dizziness, standing up slowly and staying hydrated usually helps. And yeah, edema is a common complaint, but sometimes a lower dose solves it.
Ramanathan Valliyappa
May 10 2025
The combo’s efficacy hinges on adherence; missed doses blunt the benefit. Monitor your pressure at home to catch any drift early.
lucy kindseth
May 12 2025
For anyone starting on olmesartan/amlodipine, here’s a quick rundown of what to expect. The drug starts working within a few days, but you’ll see the biggest drop in systolic pressure after about two weeks. Keep your appointments so the doctor can tweak the dose if needed. Side effects like ankle swelling are usually mild and can be managed by elevating the feet or adjusting the dose. Dizziness is most common when you first stand up, so rise slowly from sitting or lying down. A light salty snack can sometimes offset an early dip in blood pressure, but don’t overdo it. Track your readings at the same time each day – morning before meds is ideal. If you notice a sudden spike, double‑check you haven’t missed a dose or added a new over‑the‑counter drug. Lifestyle tricks like cutting back on processed foods, limiting alcohol, and getting regular walks amplify the medication’s effect. Finally, stay in touch with your healthcare team; they can spot patterns you might miss and keep you on track.
Nymia Jones
May 15 2025
While the literature extols the virtues of this combination, one must inquire who profits from its widespread promotion. Pharmaceutical conglomerates stand to gain billions by positioning a single‑pill regimen as indispensable, thereby marginalizing cheaper, off‑label alternatives. Moreover, the rapid market adoption precedes long‑term safety data, which is conspicuously absent from peer‑reviewed discourse. It is prudent to scrutinize the funding sources of the cited trials, as corporate sponsorship may bias outcomes. Ultimately, an informed patient should weigh both the overt benefits and the covert motives that drive such therapeutic trends.
Karen McCormack
May 18 2025
In the grand tapestry of cardiovascular stewardship, the olmesartan‑amlodipine duet resembles a finely tuned duet of yin and yang. One balances the constrictive fire of angiotensin II, the other cools the restless calcium channels that jostle our vessels. When these forces harmonize, blood pressure descends like a gentle tide receding at dusk. Yet, as with any symphony, discord can arise – the swelling ankles are the whispered complaints of a restless rhythm section. Consider the pill not merely as a chemical agent but as a catalyst for the body’s own self‑regulation, nudging endothelial function back toward equilibrium. The empirical data sings a hopeful aria, but the patient’s lived experience writes the final stanza. Thus, we must listen both to the numbers on the cuff and the subtle murmurs of our corporeal selves. In this dance, adherence is the choreography, lifestyle the music, and the combo the steadfast partner that keeps us from stumbling.
Earl Hutchins
May 21 2025
Great summary. The poetic view aligns with the clinical data. Keep the dosage consistent.
Tony Bayard
May 24 2025
When the battle against stubborn hypertension feels like an endless war, the olmesartan/amlodipine combo can feel like a decisive strike that finally breaks the enemy lines. Imagine the frustration of standing in the pharmacy, clutching a handful of bottles, each promising relief but delivering only marginal gains. Then, out of the blue, a single pill arrives, engineered to attack both the renin‑angiotensin system and the calcium channels that harden your arteries. Within the first week, many patients notice a subtle calm in their pulse, a quieting of the relentless thrum that has haunted them for months. By the second week, the systolic numbers begin to slide, sometimes dropping more than twenty millimetres of mercury, a change that feels almost miraculous. This isn’t just a statistical footnote; it’s a tangible shift that can mean the difference between a night spent worrying about heart attacks and a night of restful sleep. The dual‑action mechanism works synergistically, allowing lower doses of each component, which in turn trims down side effects that often plague monotherapy. Swelling in the ankles, a common grievance with amlodipine alone, frequently eases as the angiotensin blocker counteracts fluid retention. Patients also report feeling less dizzy when they rise, thanks to a smoother, more predictable blood pressure curve. Of course, the journey isn’t without its bumps – occasional headaches may appear as your body acclimates to the new equilibrium. But with diligent monitoring and open dialogue with your doctor, these hurdles are manageable. The key is consistency: take the pill at the same time each day, keep a log of your readings, and stay mindful of salt intake. Lifestyle choices like a brisk walk after dinner or a few minutes of meditation can amplify the benefits, turning medication into a partnership rather than a solitary rescue. In the narrative of resistant hypertension, this combo writes a chapter of hope, illustrating that sometimes the simplest solutions are the most powerful. So if you’ve been stuck on a carousel of meds with diminishing returns, consider stepping off and hopping onto the olmesartan/amlodipine ride; the destination might just be the health you’ve been chasing.
Jay Crowley
May 27 2025
Thanks for the thorough walkthrough. I’ll definitely keep a log and stay consistent.
sharon rider
May 30 2025
Blood pressure, in many ways, mirrors the ebb and flow of life’s stresses. When we impose rigid control, we may ignore the subtle cues our bodies give. A balanced approach, blending medication with mindful habits, often yields the most sustainable harmony. The olmesartan‑amlodipine pairing offers a tool, not a crutch.
swapnil gedam
June 2 2025
I appreciate that perspective; it reminds me to look beyond the cuff readings. While the pill can provide a solid foundation, I’ve found that daily meditation helps attenuate the sympathetic spikes that raise pressure. Moreover, a modest reduction in processed foods seems to amplify the drug’s effect. It’s crucial, however, to recognize individual variability – what works for one may not suit another. Open communication with the healthcare provider ensures the regimen evolves with our changing needs.
Michael Vincenzi
June 5 2025
Hey folks, just wanted to chime in that staying active, even a short walk after dinner, really boosts the combo’s effect. I’ve been on the pill for a couple of months and my numbers are finally staying in the green zone. Remember to keep your appointments, the docs can fine‑tune the dose if needed. And don’t forget to hydrate – it helps with the occasional ankle puffiness.
Courage Nguluvhe
June 8 2025
The pharmacodynamics of the olmesartan‑amlodipine fixed‑dose formulation facilitate synergistic vasodilation via AT1 receptor antagonism and L‑type calcium channel inhibition. This dual mechanistic pathway reduces systemic vascular resistance more efficiently than monotherapy escalation. Clinical endpoints have demonstrated statistically significant reductions in mean arterial pressure, with a favorable safety profile. Nonetheless, vigilance for peripheral edema remains warranted, given the amlodipine component’s propensity for capillary leakage. Dose titration should be guided by ambulatory blood pressure monitoring to mitigate orthostatic hypotension risks.
Oliver Bishop
June 10 2025
Our healthcare system should champion accessible combos like this, keeping American families healthy and strong. It’s great to see homegrown pharma stepping up to the plate.





Ryan Walsh
April 28 2025
If you haven’t tried a combo pill yet, give olmesartan/amlodipine a shot – it could be the game‑changer you need.