Warfarin and Ibuprofen: Risks, Interactions, and Safer Pain Relief Options
When you're taking warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it works by slowing down your body’s ability to form clots. But if you reach for a common pain reliever like ibuprofen, a nonsteroidal anti-inflammatory drug (NSAID) sold under brands like Advil or Motrin. Also known as NSAID, it reduces pain and swelling by blocking certain enzymes, you might be putting yourself at serious risk. Mixing these two isn’t just a minor concern—it can lead to internal bleeding, hospital visits, or worse. This isn’t a myth. Studies show that people on warfarin who regularly take ibuprofen have up to a 30% higher chance of major bleeding compared to those who avoid NSAIDs.
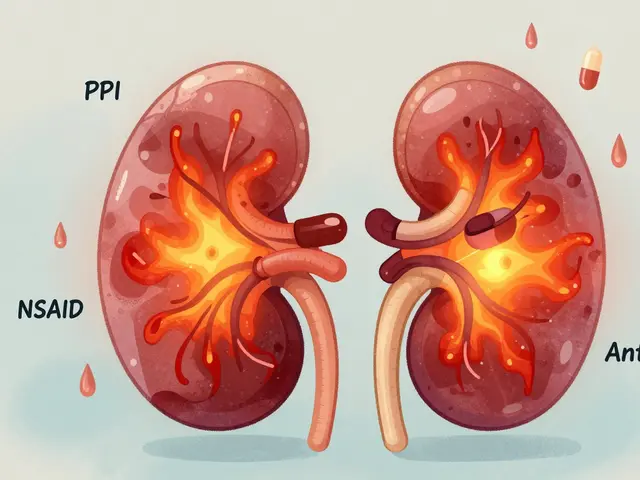
Why does this happen? Warfarin makes your blood take longer to clot. Ibuprofen irritates the stomach lining and also interferes with platelets—the tiny blood cells that help stop bleeding. Together, they create a double threat: more bleeding from the gut and slower clotting overall. Even a single dose can be risky if you’re already on a high warfarin dose or have other health issues like ulcers, kidney problems, or high blood pressure. And here’s the kicker: many people don’t realize ibuprofen is in cold medicines, menstrual relief pills, or even topical gels. That sneaky ingredient can sneak in without you knowing.
So what can you do instead? acetaminophen, the active ingredient in Tylenol. Also known as paracetamol, it’s generally considered the safest pain reliever for people on warfarin—as long as you stick to the recommended dose (no more than 3,000 mg a day). It doesn’t affect clotting or stomach lining like NSAIDs do. For inflammation, talk to your doctor about alternatives like physical therapy, heat packs, or low-dose corticosteroids if needed. Some people find relief with topical capsaicin or fish oil supplements, but always check with your provider first. Don’t assume natural means safe—some herbs like garlic, ginger, or ginkgo can also thin your blood.
Regular blood tests (INR checks) are your safety net. If you start or stop any new medication—even over-the-counter ones—tell your doctor. Keep a list of everything you take, including supplements. If you notice unusual bruising, nosebleeds, dark stools, or sudden headaches, don’t wait. These could be early signs of bleeding. The goal isn’t to avoid pain relief entirely—it’s to choose the right kind. You don’t have to suffer, but you do need to be smart.
Below, you’ll find real comparisons of pain relievers, blood thinners, and safe alternatives that people actually use. No guesswork. No fluff. Just clear, practical info to help you stay safe and in control.

Heart Medications and Their Dangerous Combinations: What to Avoid
Heart medications can save lives-but dangerous combinations with NSAIDs, blood thinners, or supplements can cause bleeding, heart failure, or death. Learn the top 7 risky combos and how to stay safe.
View More