Sleep Apnea Medication Risk: Key Facts You Should Know
If you’ve been prescribed medication for sleep apnea, you’re probably wondering whether the benefits outweigh the downsides. Most people think of CPAP machines first, but doctors also use drugs like modafinil, armodafinil, and certain nasal sprays to help you stay awake during the day or keep your airway open at night. These medicines can be a game‑changer, yet they come with their own set of risks that many patients overlook.
Common Sleep Apnea Drugs and Their Side Effects
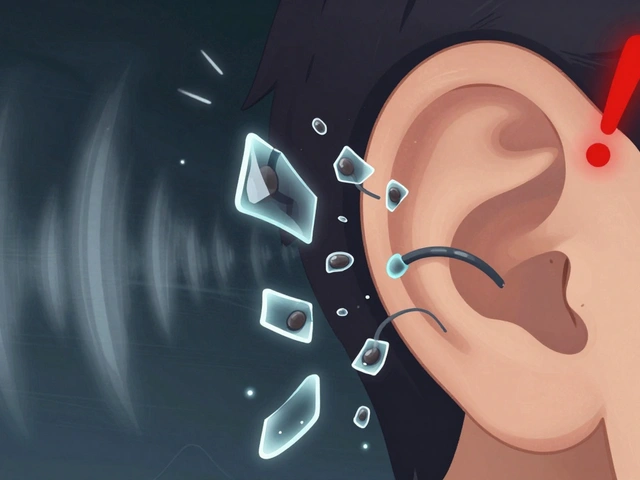
Modafinil and armodafinil are the most popular wake‑promoting agents for people with obstructive sleep apnea. They can improve daytime alertness, but they may also cause headaches, nausea, anxiety, or a rapid heartbeat. Some users report sudden mood swings or trouble sleeping even more. Nasal decongestants like oxymetazoline or phenylephrine shrink swollen tissue in the nose, but overuse can lead to rebound congestion, high blood pressure, and heart palpitations.
Other prescriptions include certain antidepressants (like trazodone) that help with sleep quality. While they can be effective, they sometimes cause dizziness, dry mouth, or an increased risk of falls, especially in older adults. If you’re on a blood thinner, be aware that some sleep apnea meds can interact and raise bleeding risk.
How to Reduce Risks and Stay Safe
The best way to keep medication risks low is to start low and go slow. Begin with the smallest dose your doctor suggests and let your body adjust before increasing it. Keep a simple diary of any new symptoms—headaches, jitteriness, or changes in blood pressure—so you can spot patterns early.
Never mix sleep apnea pills with alcohol or recreational drugs. Alcohol can amplify sedative effects and make breathing problems worse. If you take over‑the‑counter antihistamines for allergies, check with your pharmacist because many of them can make you drowsy or interact with wake‑promoting meds.
Regular check‑ups are crucial. Ask your doctor to review your medication list at least every six months, especially if you add new prescriptions for unrelated conditions. Blood pressure checks, liver function tests, and a quick eye on your heart rhythm can catch side effects before they become serious.
Finally, consider non‑drug alternatives as part of your treatment plan. Weight management, positional therapy (sleeping on your side), and consistent use of a properly fitted CPAP mask often reduce the need for high‑dose medications. Combining lifestyle changes with the right drug can give you the best of both worlds—fewer side effects and better sleep quality.
In short, sleep apnea meds can help you stay awake and feel better, but they’re not risk‑free. By staying informed, tracking how you feel, and keeping an open line with your healthcare team, you can enjoy the benefits while keeping the downsides in check.

Ropinirole and Sleep Apnea: Essential Facts for Patients
Learn how Ropinirole may affect sleep apnea, the signs to watch for, and practical steps to stay safe while treating Parkinson's or restless legs syndrome.
View More