
Inhaler Comparison Tool
Compare key features of inhalers for asthma and COPD to find the best match for your needs.
Personal Profile
Recommended Inhaler
Symbicort is a combination inhaler that contains budesonide, a corticosteroid, and formoterol, a long‑acting β2‑agonist (LABA). It’s prescribed for moderate‑to‑severe asthma and COPD, delivering both anti‑inflammatory and bronchodilatory action in a single puff. While the dual‑action formula works well for many, patients often wonder if other inhalers might suit their lifestyle, budget, or side‑effect profile better. This article breaks down the most common alternatives, compares key attributes, and helps you decide which device aligns with your breathing needs.
Why Compare Inhalers?
Asthma and COPD aren’t one‑size‑fits‑all. Age, inhaler technique, comorbidities, and cost all influence adherence. Switching to a different inhaler can improve symptom control, reduce exacerbations, or simply make daily use less of a chore. Below we’ll explore the clinical differences, device ergonomics, and practical considerations that matter to patients and prescribers alike.
Core Entities and Their Attributes
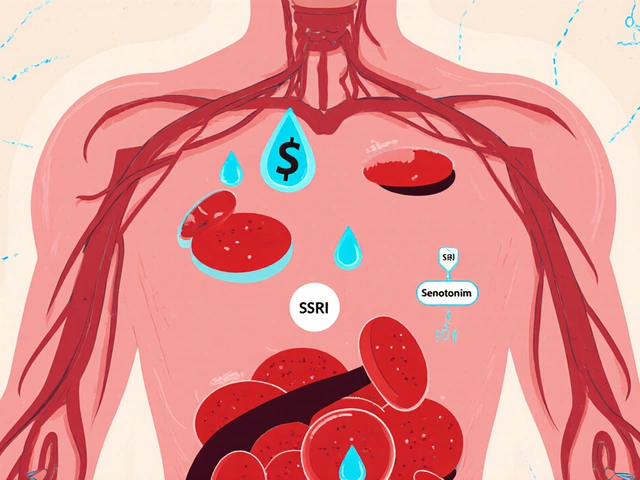
- Budesonide is an inhaled corticosteroid (ICS) that reduces airway inflammation, with a typical dose of 200‑400µg per inhalation.
- Formoterol is a LABA that provides rapid bronchodilation (within minutes) and lasts up to 12hours.
- Advair combines fluticasone propionate (ICS) with salmeterol (LABA) in a dry‑powder inhaler, approved for asthma and COPD.
- Pulmicort delivers budesonide alone via a nebuliser‑type inhaler, ideal for children or patients with poor hand‑breath coordination.
- Breo Ellipta pairs fluticasone furoate with vilanterol, offering once‑daily dosing for asthma and COPD.
- Spiriva contains tiotropium, a long‑acting muscarinic antagonist (LAMA) used once daily for COPD maintenance.
- Dulera merges mometasone (ICS) with formoterol (LABA) in a metered‑dose inhaler (MDI) for patients needing a lower‑dose combination.
- Albuterol is a short‑acting β2‑agonist (SABA) used for quick relief of acute bronchospasm.
Comparison Table: Symbicort vs. Leading Alternatives
| Product | Active Ingredients | Indication | Device Type | Typical Price (UK) | Dosage Frequency |
|---|---|---|---|---|---|
| Symbicort | Budesonide/Formoterol | Asthma, COPD | MDI (press‑and‑burst) | ≈£35-£40 | Twice daily |
| Advair Diskus | Fluticasone/Salmeterol | Asthma, COPD | Dry‑powder inhaler | ≈£45-£50 | Twice daily |
| Breo Ellipta | Fluticasone/Vilanterol | Asthma, COPD | Ellipta DPI | ≈£55-£60 | Once daily |
| Dulera | Mometasone/Formoterol | Asthma (moderate) | MDI | ≈£30-£35 | Twice daily |
| Pulmicort Respules | Budesonide (ICS only) | Asthma (mild‑moderate), pediatric | Nebuliser‑type inhaler | ≈£20-£25 | Twice daily |
How to Pick the Right Inhaler for You
Think of inhaler choice like picking a pair of shoes-you need the right fit, comfort, and support for the terrain you walk on. Below are the decision criteria most clinicians and patients weigh.
- Efficacy for your disease stage. For patients who need both anti‑inflammatory and bronchodilator action, a fixed‑dose combination (FDC) such as Symbicort, Advair, or Dulera is usually first‑line.
- Device handling skills. MDIs require coordinated inhalation; dry‑powder inhalers (DPIs) depend on a strong inspiratory flow. If hand‑breath coordination is a challenge, a nebuliser‑type inhaler like Pulmicort may be safer.
- Dosing convenience. Once‑daily options (Breo Ellipta) reduce pill‑burden and improve adherence, especially for elderly patients.
- Side‑effect profile. High‑dose steroids increase risk of oral thrush and dysphonia. Formoterol has a faster onset than salmeterol, which can be useful for quick relief but may cause tremor in sensitive individuals.
- Cost and NHS availability. While most inhalers are available on the NHS, private prescriptions can vary. Symbicort’s price sits in the mid‑range; Breo Ellipta is pricier but may qualify for special funding in severe cases.
Real‑World Scenarios
Imagine Sarah, a 68‑year‑old with COPD who struggles to generate enough inspiratory flow for a DPI. Her doctor switched her from Breo Ellipta to Symbicort because the MDI’s spray can be activated with a simple press, making inhalation easier. After three months, Sarah reported fewer exacerbations and a noticeable drop in night‑time coughing.
Contrast that with James, a 25‑year‑old athlete with mild‑persistent asthma. He prefers a once‑daily inhaler to avoid interrupting training. After trialing Budesonide alone (Pulmicort) and still experiencing occasional wheeze, he moved to Budesonide/Formoterol in a DPI (Symbicort) and found the rapid bronchodilation helped during high‑intensity workouts.
Safety and Common Concerns
All inhaled corticosteroids carry a small risk of oral candidiasis. Rinsing the mouth with water after each use dramatically cuts that risk-something patients often overlook. Formoterol, like other LABAs, should never be used as monotherapy for asthma because it can mask worsening inflammation; always pair it with an ICS, which is exactly what Symbicort does.
Another myth: “More inhalations = better control.” In reality, excess dosing can lead to systemic steroid exposure, raising concerns about bone density and glucose intolerance. Stick to the prescribed regimen and use a rescue inhaler (albuterol) for breakthrough symptoms.
Connected Topics Worth Exploring
If you’re digging into inhaler options, you’ll likely encounter these related concepts:
- Asthma action plan - a written guide that outlines daily medication, trigger avoidance, and steps for worsening symptoms.
- COPD phenotypes - emphysema‑dominant vs. bronchitis‑dominant, influencing inhaler choice.
- Adherence monitoring - smart inhalers and pharmacy refill data help clinicians spot non‑compliance.
- Inhaler technique training - videos, face‑to‑face coaching, or apps that guide patients through proper use.
Each of these topics deepens your understanding of why the right inhaler matters beyond the drug’s chemistry.
Bottom Line: When Symbicort alternatives Make Sense
If you need a twice‑daily regimen, have good hand‑breath coordination, and want a proven combo of steroid and fast‑acting LABA, Symbicort remains a solid choice. Switch to an alternative when:
- You struggle with the MDI technique (consider a DPI like Advair or Breo).
- Once‑daily dosing would boost adherence (Breo Ellipta).
- You require a lower steroid dose (Dulera) or prefer an inhaled steroid only (Pulmicort).
- Cost is a primary barrier and a generic version of budesonide/formoterol becomes available.
Always discuss any change with your respiratory consultant-individual response varies, and a tailored approach yields the best breath.
Frequently Asked Questions
What makes Symbicort different from Advair?
Symbicort pairs budesonide with formoterol, while Advair combines fluticasone with salmeterol. Formoterol has a quicker onset (minutes) compared with salmeterol’s slower onset (10‑20 minutes). Budesonide also has a slightly higher lung‑deposition efficiency, which may translate to lower systemic exposure for the same anti‑inflammatory effect.
Can I use Symbicort as a rescue inhaler?
No. Although formoterol provides rapid relief, guidelines advise a dedicated short‑acting bronchodilator (e.g., albuterol) for rescue because a LABA alone can mask worsening inflammation.
Is a generic version of budesonide/formoterol available?
Yes, several manufacturers have launched generic inhalers in Europe and the UK. Prices are typically 15‑25% lower than the branded Symbicort, but device ergonomics may differ, so discuss with your pharmacist.
What side‑effects should I watch for?
Common issues include oral thrush, hoarse voice, and mild tremor after dosing. Rinsing the mouth, using a spacer, and timing the inhaler away from bedtime can minimize these effects.
How do I know if I’m using the inhaler correctly?
A correct technique yields a visible plume and no coughing immediately after inhalation. Ask your GP or pharmacist for a quick demonstration, or use a checklist: shake, exhale fully, place mouthpiece, inhale slowly (MDI) or forcefully (DPI), hold breath 10 seconds, then exhale.
12 Comments
Daisy canales
October 2 2025
Wow, another giant table for us to stare at. So helpful that nobody actually reads the fine print.
keyul prajapati
October 8 2025
When it comes to selecting an inhaler, the decision matrix is rarely a simple tick‑box exercise. Patients must first assess the severity of their airway disease, distinguishing between intermittent, mild‑persistent, and severe‑persistent patterns. The presence of comorbidities such as heart failure or diabetes can influence the choice of corticosteroid dose, given the systemic absorption risk. Hand‑breath coordination is another critical factor; individuals with arthritis or reduced dexterity often struggle with the forced inhalation required by dry‑powder inhalers. In such scenarios, a metered‑dose inhaler (MDI) equipped with a spacer can dramatically improve drug delivery. Budget constraints play a non‑trivial role, especially in health systems where co‑payments vary widely; generic budesonide/formoterol options may reduce expenditures by up to a quarter compared with brand‑name products. Frequency of dosing also matters: once‑daily formulations like Breo Ellipta have been shown to increase adherence in elderly populations, whereas twice‑daily regimens may be preferable for those who require tighter symptom control. The adverse‑effect profile should never be ignored-higher‑dose inhaled steroids increase the likelihood of oral candidiasis, so mouth‑rinsing after each use is a best‑practice recommendation. Moreover, LABA components such as formoterol provide rapid bronchodilation, but they must always be paired with an inhaled corticosteroid to avoid unchecked inflammation. Patient education, including proper inhaler technique training, can cut exacerbation rates by up to 30 %. Finally, clinicians should regularly review inhaler technique at each visit, as errors often develop over time despite initial instruction. In summary, the optimal inhaler is the one that aligns with the patient’s disease severity, physical ability, financial situation, and lifestyle preferences while minimizing side effects.
Alice L
October 13 2025
While the preceding remarks are thorough, it is worth noting that cultural considerations occasionally affect device preference; certain populations exhibit a higher comfort level with press‑and‑burst mechanisms due to prior exposure in community health programs.
Seth Angel Chi
October 19 2025
Honestly the whole Symbicort hype is overrated.
Ralph Louis
October 24 2025
Overrated? Please. You’re ignoring the pharmacokinetic edge that budesonide offers-higher lung‑deposit, lower systemic load. That’s why clinicians keep prescribing it despite the marketing hype.
Olivia Christensen
October 30 2025
Totally get how overwhelming this can be 😊. If you’re not sure which device feels right, try a demo at your pharmacy; feeling confident with the inhaler can make a huge difference in day‑to‑day comfort.
Lauren W
November 4 2025
Indeed, the tactile feedback of an MDI, the audible click of a DPI, and even the subtle resistance of a nebuliser each convey unique cues-as such, a brief, hands‑on trial can illuminate personal preference, mitigating the risk of future non‑adherence, which, as you know, is a leading cause of exacerbations.
Justin Valois
November 10 2025
All this science talk is just a distraction from the truth-our lungs belong to the nation, not to multinational pharma.
Ryan Smith
November 15 2025
Sure, because Big Pharma is secretly running the government’s air‑quality program. Got any evidence?
Ash Charles
November 21 2025
Listen up, folks-pick the inhaler that you can actually use every day, stay consistent, and you’ll see real improvement. No fluff, just results.
Michael GOUFIER
November 26 2025
In accordance with the foregoing advice, diligent adherence to a suitably selected inhaler regimen constitutes the cornerstone of optimal respiratory management.





vijay sainath
September 27 2025
Your article reads like a cheap sales pitch.