Lymphoma Sleep Disturbances: Causes, Impact, and Management
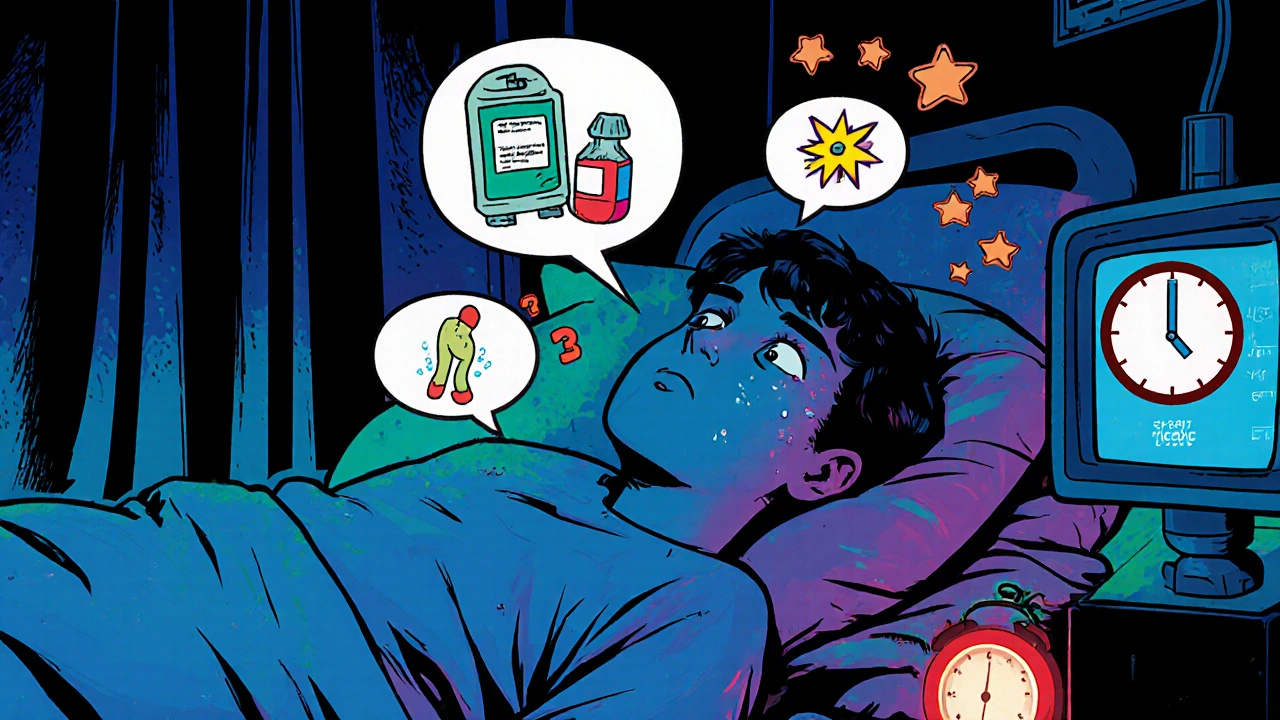
When dealing with lymphoma sleep disturbances, disruptions in sleep that many lymphoma patients experience. Also known as cancer‑related insomnia, this issue can worsen fatigue and interfere with treatment effectiveness.
Understanding lymphoma, a cancer of the lymphatic system that often requires chemotherapy or radiation is the first step. The disease itself, plus the drugs used to fight it, create a perfect storm for sleep problems. lymphoma sleep disturbances frequently manifest as difficulty falling asleep, frequent awakenings, or early morning waking. These symptoms form a feedback loop: poor sleep boosts fatigue, fatigue lowers daytime activity, and low activity reduces natural sleep drive.
Why sleep matters for lymphoma patients
Sleep isn’t just rest; it’s a critical repair phase for the immune system. For anyone undergoing chemotherapy, potent drugs that target rapidly dividing cells, quality sleep helps reduce inflammation and supports blood cell recovery. When sleep quality drops, the body’s ability to handle side effects like nausea or pain drops too. In other words, better sleep can blunt the harshest chemo side effects. That’s why clinicians often recommend sleep hygiene as part of the overall care plan.
One of the most common sleep‑related complaints is insomnia, a condition that’s distinct from occasional sleeplessness. Insomnia in the lymphoma context is often driven by heightened anxiety, pain, and the hormonal changes caused by steroids. The semantic link is clear: lymphoma sleep disturbances encompass insomnia, while anxiety and pain act as catalysts. Managing these triggers can break the cycle. Simple steps like limiting caffeine after noon, establishing a wind‑down routine, and keeping the bedroom cool can make a noticeable difference.
Another piece of the puzzle is the circadian rhythm, the body’s internal clock that tells us when to be awake or asleep. Treatments administered at night can shift this clock, leading to fragmented sleep. Studies show that aligning medication timing with natural daylight can improve sleep outcomes. So, circadian rhythm, the 24‑hour biological cycle governing sleep‑wake patterns becomes a therapeutic target. Light therapy in the morning or melatonin supplements in the evening are practical tools to reset the clock.
Fatigue is often the headline symptom patients mention, but it’s usually a downstream effect of disrupted sleep. While fatigue and sleep loss are interrelated, they’re not identical. Fatigue can linger even after a good night’s rest, especially if anemia or muscle loss accompanies the cancer. Recognizing the difference helps clinicians prescribe tailored interventions—exercise for fatigue, sleep hygiene for insomnia, and medication adjustments for both.
Beyond medical strategies, lifestyle habits play a big role. Regular gentle exercise, like short walks or yoga, boosts natural sleep drive and reduces anxiety. Nutrition matters too: heavy meals close to bedtime can cause reflux, waking you up. Hydration is important, but timing fluid intake can prevent nighttime bathroom trips. Integrating these habits into daily life gives patients more control over their sleep quality, even when other aspects of treatment feel out of reach.
Finally, support networks matter. Talking with a therapist, joining a patient support group, or simply sharing concerns with family can lower stress hormones that keep the brain wired for alertness. When emotional burdens lighten, the brain can more easily transition into sleep mode. So, the relationship between emotional health and mental well‑being, the psychological state influencing sleep and recovery is a key part of the overall plan.
All these pieces—disease biology, treatment timing, insomnia, circadian rhythm, fatigue, lifestyle, and emotional support—fit together like a puzzle. Below, you’ll find articles that dive deeper into each area, offering practical tips, detailed explanations, and real‑world advice to help you tackle lymphoma‑related sleep disturbances head‑on.
Managing Sleep Disturbances and Insomnia in Lymphoma Patients
Learn why lymphoma patients often struggle with sleep, discover non‑drug and drug strategies, and get a step‑by‑step plan to beat insomnia and improve quality of life.
View More