
Diabetes Medication Interaction Checker
Check Your Medication Interactions
This tool helps identify potentially dangerous combinations of diabetes medications based on current medical guidelines. Always consult your healthcare provider before changing medications.
Combining diabetes medications can be a powerful way to control blood sugar-but it can also be dangerous if you don’t know what you’re mixing. Some drug pairs work well together. Others? They can send your glucose levels crashing or skyrocketing without warning. The diabetes drug interactions you need to watch out for aren’t just theoretical-they’ve landed people in the ER. And with more people using multiple medications to manage type 2 diabetes, this isn’t something you can afford to ignore.
Why Some Combinations Are Risky
Not all diabetes drugs act the same way. Some lower blood sugar by making your body release more insulin. Others help your kidneys flush out excess glucose. A few even make your cells more sensitive to insulin. When you stack them, their effects don’t always add up neatly. Sometimes they clash.The biggest danger? Hypoglycemia. That’s when your blood sugar drops too low. Symptoms like shakiness, sweating, confusion, or fainting can come on fast. In older adults or those with kidney problems, this can be life-threatening. On the flip side, some drugs-like steroids or certain diuretics-can raise blood sugar so much that your diabetes meds can’t keep up. This leads to hyperglycemia, which over time damages nerves, kidneys, and blood vessels.
High-Risk Combinations to Avoid
Certain drug pairs are known troublemakers. The American Diabetes Association’s 2025 guidelines specifically warn against a few combinations.- Insulin + Rosiglitazone: This combo can cause fluid retention and worsen heart failure. Rosiglitazone (a thiazolidinedione) makes your body hold onto water. Add insulin, which also promotes fluid retention, and you’re asking for swelling in the legs, shortness of breath, or even hospitalization.
- Meglitinides + Azole Antifungals: Drugs like ketoconazole or fluconazole (used for yeast infections) block the liver enzyme CYP3A4. This is the same enzyme that breaks down repaglinide and nateglinide. When it’s blocked, these drugs build up in your blood, causing severe, prolonged hypoglycemia-even if you haven’t changed your dose.
- DPP-4 Inhibitors + GLP-1 RAs: These two work the same way. Both boost GLP-1, a hormone that helps your pancreas release insulin. Using them together doesn’t improve control-it just increases side effects like nausea and pancreatitis risk. The ADA explicitly says this combo should never be used.
Even common medications can interfere. Quinine (used for leg cramps) can trigger hypoglycemia. Corticosteroids (like prednisone) can spike blood sugar so high that even insulin doesn’t help. If you’re on one of these, check your glucose more often. Don’t assume your diabetes meds are still doing their job.
What Makes a Safer Combination?
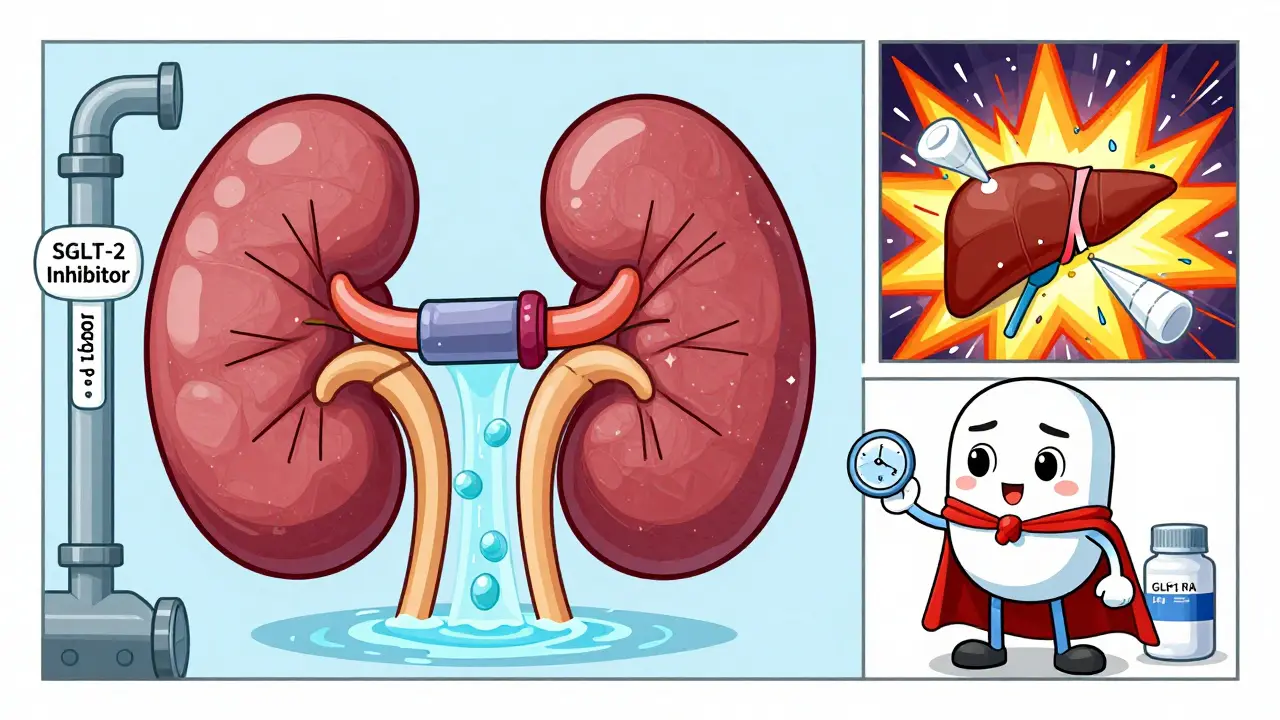
Not all newer diabetes drugs come with baggage. In fact, two of the most recent classes are among the safest to combine with others.GLP-1 receptor agonists (like semaglutide or liraglutide) lower blood sugar without causing much hypoglycemia. They work by triggering insulin release only when glucose is high-so they’re less likely to crash your levels. They also help with weight loss and reduce heart risks. That’s why combining a GLP-1 RA with insulin is now preferred over insulin alone for many people. It gives better control with fewer lows.
SGLT-2 inhibitors (like empagliflozin or dapagliflozin) work in the kidneys. They make your body pee out extra sugar. Since they don’t rely on insulin, they rarely cause hypoglycemia-even when paired with insulin or sulfonylureas. They also protect the heart and kidneys. That’s why doctors now often add an SGLT-2 inhibitor to a patient’s regimen instead of adding another insulin dose.
How Your Body Processes These Drugs
The real hidden risk? Your liver and kidneys. Most diabetes drugs are broken down by liver enzymes-especially CYP3A4, CYP2C9, and CYP2C8. If another drug blocks or speeds up these enzymes, your diabetes medication’s level in your blood changes.- Repaglinide (a meglitinide) is mainly broken down by CYP3A4 and CYP2C8. If you take it with clarithromycin (an antibiotic) or itraconazole (an antifungal), your repaglinide levels can spike. Result? Severe hypoglycemia.
- Nateglinide is processed by CYP2C9. Drugs like fluconazole or warfarin can interfere here too.
- Sulfonylureas (like glimepiride) also use CYP2C9. So can a common painkiller like celecoxib. It’s not always obvious.
Metformin is different. It doesn’t go through the liver much. But it’s cleared by the kidneys. If you have kidney problems-or you’re taking a drug that affects kidney function (like contrast dye or NSAIDs)-metformin can build up. This raises the risk of lactic acidosis, a rare but serious condition.

What You Should Do
If you’re on more than one diabetes drug, here’s what to do right now:- Review all your meds-including OTC drugs, supplements, and antibiotics. A single pill for a yeast infection can change everything.
- Monitor your blood sugar more often for the first week after starting or changing any drug. Look for patterns: Are your numbers dropping at night? Spiking after meals?
- Know your warning signs. If you feel dizzy, sweaty, or confused, check your glucose. Don’t wait.
- Talk to your pharmacist. They’re trained to spot drug interactions. Bring a full list of everything you take, even herbal teas.
- Ask about alternatives. If you’re on a risky combo, ask if switching to a GLP-1 RA or SGLT-2 inhibitor could reduce your risk.
There’s no one-size-fits-all plan. But the goal is simple: keep your blood sugar steady, avoid hospital visits, and protect your long-term health. The safest combinations aren’t always the most familiar ones. Sometimes, the best move is to drop a drug that’s been in your regimen for years-and replace it with something newer, safer, and better studied.
What’s Coming Next
Researchers are now looking at how transporter proteins like P-glycoprotein affect diabetes drugs. These proteins help move drugs in and out of cells. If a drug blocks them, it can change how your body absorbs or clears medications. Early studies suggest DPP-4 inhibitors like sitagliptin might be affected. This could explain why some people suddenly have low blood sugar even without dose changes.For now, stick to the basics: know your drugs, watch your numbers, and don’t assume everything is safe just because your doctor prescribed it. The science is moving fast-but your safety doesn’t have to be a gamble.
Can I take over-the-counter painkillers with my diabetes meds?
Some OTC painkillers can interfere. NSAIDs like ibuprofen or naproxen may increase the risk of low blood sugar when taken with sulfonylureas. Acetaminophen is usually safer, but it can interfere with some glucose monitors. Always check with your pharmacist before using any OTC pain reliever regularly.
Is it safe to combine insulin with GLP-1 RAs?
Yes, and it’s often recommended. Combining insulin with a GLP-1 RA gives better blood sugar control than insulin alone, with fewer episodes of low blood sugar. It also helps with weight loss and reduces heart disease risk. This combo is now a first-line option for many people with type 2 diabetes who need more than one drug.
Why are SGLT-2 inhibitors considered safer than older drugs?
SGLT-2 inhibitors lower blood sugar by making your kidneys remove excess glucose through urine. They don’t rely on insulin or liver enzymes, so they rarely cause hypoglycemia-even when taken with insulin or sulfonylureas. They also protect the heart and kidneys, making them a preferred add-on for people with cardiovascular or kidney disease.
Can antibiotics cause low blood sugar in diabetics?
Yes, especially azole antifungals (like fluconazole) and certain antibiotics like clarithromycin. These block liver enzymes that break down meglitinides and sulfonylureas, causing them to build up. This can lead to dangerous hypoglycemia. Always tell your doctor you have diabetes before starting any new antibiotic or antifungal.
Should I stop my diabetes meds before surgery?
Never stop without medical advice. Some drugs, like metformin, may need to be paused before surgery due to kidney stress from contrast dye. Others, like SGLT-2 inhibitors, increase the risk of ketoacidosis during fasting. Your care team will give you specific instructions based on your meds and the type of surgery.





