When you’re traveling abroad and something goes wrong-maybe you get sick, have an accident, or suffer an allergic reaction-your body can’t speak the local language. But your medications can. If you don’t have a clear, printed list of what you’re taking, in a language the doctor understands, you could face delays, wrong treatments, or even dangerous mistakes. This isn’t theoretical. In 2020, a study in JAMA Internal Medicine found that patients who carried a multilingual medication list had 28% fewer medication errors during hospital admissions. That’s not just convenience. That’s life or death.
Why a multilingual medication list matters
Every year, over 25 million people in the U.S. alone have limited English proficiency. Many of them travel. Others live abroad, work overseas, or visit family in countries where English isn’t spoken. In an emergency, you might not be able to say your name, let alone explain that you take 5 mg of warfarin every Monday, Wednesday, and Friday. Emergency rooms in London, Tokyo, or Mexico City don’t have time to guess. They need facts fast. Without a translated list, staff might miss a drug interaction, give you a medication you’re allergic to, or repeat a dose you already took. A 2021 study showed that language barriers increase adverse drug events by 35%. That’s why a simple printed list, in your native language and the language of the country you’re visiting, can cut emergency room time by over 20 minutes.What to include on your list
A good multilingual medication list isn’t just a copy of your prescription bottle. It needs to be clear, complete, and consistent. Here’s what to write down:- Medication name - Use the generic name (like metformin), not the brand (like Glucophage). Generic names are the same worldwide.
- Dosage - How much you take (e.g., 500 mg).
- Frequency - How often (e.g., once daily, twice a week).
- Purpose - Why you take it (e.g., “for high blood pressure,” “for type 2 diabetes”).
- Prescribing doctor - Name and clinic, so they can verify if needed.
- Start date - When you began taking it.
- Supplements and herbs - Things like fish oil, garlic pills, or traditional remedies. These are often missed but can cause serious interactions.
Don’t forget over-the-counter drugs, vitamins, or even herbal teas you take daily. A 2022 survey found that 52% of non-English speakers were taking herbal medicines not listed on their forms-because they didn’t think they counted.
Where to get translations
You don’t need to hire a translator. Several trusted organizations already offer free, medically accurate multilingual lists.- Tennessee Pharmacists Association (TPA) Universal Medication List - Available in 10 languages: English, Spanish, Chinese, Vietnamese, Korean, Arabic, Russian, Somali, Nepali, and French. It’s printable, free, and used by hospitals across the U.S. You can download it from their website.
- NPS MedicineWise app - Originally from Australia, this app lets you enter your meds, set reminders, and switch the interface to 11 languages including Arabic, Hindi, Persian, and Vietnamese. It syncs across phones and lets you email or print a list. It’s free on iOS and Android.
- MedlinePlus - Run by the U.S. National Library of Medicine, this site offers medication guides in over 40 languages. While it doesn’t let you create a personal list, you can use their templates to build your own.
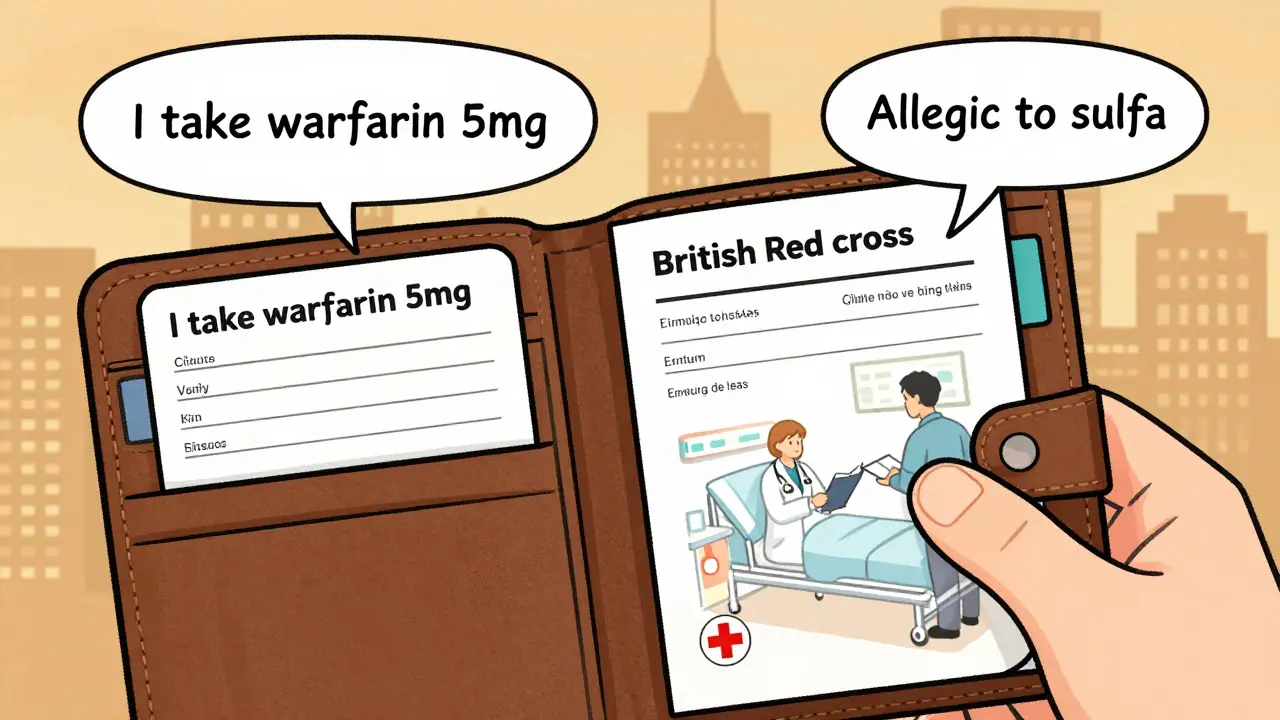
- British Red Cross Emergency Phrasebook - This isn’t a medication list, but it’s the best tool for communicating in an emergency. It includes 150+ medical phrases translated into 36 languages. You can print the section on medications and carry it with your list.
For example: If you’re from Vietnam and traveling to Germany, download the Vietnamese version of the TPA list and the German version of the Red Cross phrasebook. Put them together in a plastic sleeve inside your wallet.
How to use it in an emergency
Carrying the list isn’t enough. You need to make sure it’s used.- Keep it physical - Digital files on your phone can die. Print two copies. Put one in your wallet. Put the other in your luggage. If you’re flying, keep one in your carry-on.
- Use a clear format - Use bold headings. Leave space between each medication. No cursive handwriting. Stick to block letters.
- Teach someone - If you’re traveling with a friend or family member, show them how to hand the list to a nurse. Say: “If I can’t speak, give this to the doctor.”
- Update it every time - Every time your doctor changes your dose or adds a new drug, update the list. A 2022 study found that 78% of medication errors happen during transitions of care-like after a doctor’s visit.
One woman in Chicago told her story on Reddit: She had an allergic reaction and couldn’t speak. The ER nurse saw her Spanish-language list, spotted the penicillin allergy, and stopped the treatment before it was too late. She said her primary care doctor gave her the list during her last checkup. That’s all it took.
What to avoid
Not all translations are equal. Here’s what goes wrong:- Using Google Translate - It doesn’t know medical terms. “Take once daily” might become “Take one time every day” or worse, “Take one pill for death.”
- Only using English - Even if you speak English, you might not be able to during a panic attack or stroke.
- Leaving out herbal meds - Many cultures use traditional remedies. If you take turmeric, ginseng, or ashwagandha, include them. They can interfere with blood thinners and anesthesia.
- Using outdated versions - If your list says “2021” and you started a new drug in 2025, it’s useless.
A doctor in Ohio reported three near-misses in one month because patients brought lists with translations from their home countries. One used “heart pill” instead of “amlodipine.” Another wrote “3 times a day” but meant “every 8 hours.” Translation isn’t just about words-it’s about meaning.
What’s new in 2026
The tools are getting better. In January 2024, the CDC added medication safety guides in eight new languages, including Amharic, Hmong, and Oromo, to help refugees and displaced communities. Google now shows translated medication info directly in search results for over 100 common drugs in 30 languages. And in late 2025, the American Pharmacists Association will release the first national standard for multilingual medication lists, requiring pharmacies to offer them in languages that match their local patient population.For now, the best system is still simple: print, update, carry, and share.
Quick checklist: Your multilingual medication list
- ☑️ Generic names only
- ☑️ Dosage, frequency, purpose, doctor, start date
- ☑️ Includes supplements and herbs
- ☑️ Printed in your language + one other (e.g., English + Spanish)
- ☑️ Carried in wallet and luggage
- ☑️ Updated after every doctor visit
- ☑️ Shown to travel companion
Can I use Google Translate to make my medication list?
No. Google Translate often gets medical terms wrong. For example, it might translate “take with food” as “take with meal” or “take with death.” Use official sources like the Tennessee Pharmacists Association list or MedlinePlus. They’re reviewed by pharmacists and tested for accuracy.
What if my language isn’t on the list?
If your language isn’t available, ask your pharmacist. Many pharmacies have access to professional medical translation services. You can also use the British Red Cross Phrasebook to write down your meds manually in simple phrases: “I take [name] [dose] [time].” Then have a trusted person help you translate it into the local language. Even a handwritten note is better than nothing.
Do I need a list if I’m only traveling for a few days?
Yes. Emergencies don’t care about trip length. A fall, allergic reaction, or sudden illness can happen anytime. Over 60% of medication errors in travelers happen during short trips because people assume they’re “just visiting” and skip precautions.
Can I store my list on my phone?
You can, but don’t rely on it alone. Phones die. Screens crack. You might not be able to unlock it if you’re unconscious. Always carry a printed copy. Use the app as a backup, not your main tool.
How often should I update my list?
Update it every time your doctor changes your meds-even a small dose change. Studies show that 78% of errors happen during transitions of care, like after a hospital visit or new prescription. Make it part of your routine: update it the day after your checkup.